Antipsychotics and QT-Prolonging Drugs: What You Need to Know About Arrhythmia Risk
 Dec, 4 2025
Dec, 4 2025
QT Prolongation Risk Calculator
Assess your risk of dangerous heart rhythm problems based on medications, age, and other factors. This tool follows clinical guidelines from the article.
Enter your details to see your risk assessment
When you're taking an antipsychotic for schizophrenia, bipolar disorder, or severe depression, your mind might feel clearer-but your heart could be under silent stress. Many of these medications don’t just affect brain chemistry. They can also mess with the electrical rhythm of your heart, especially when mixed with other common drugs. This isn’t theoretical. It’s happening in clinics, hospitals, and homes right now. And the risk doesn’t just add up-it multiplies.
What Exactly Is QT Prolongation?
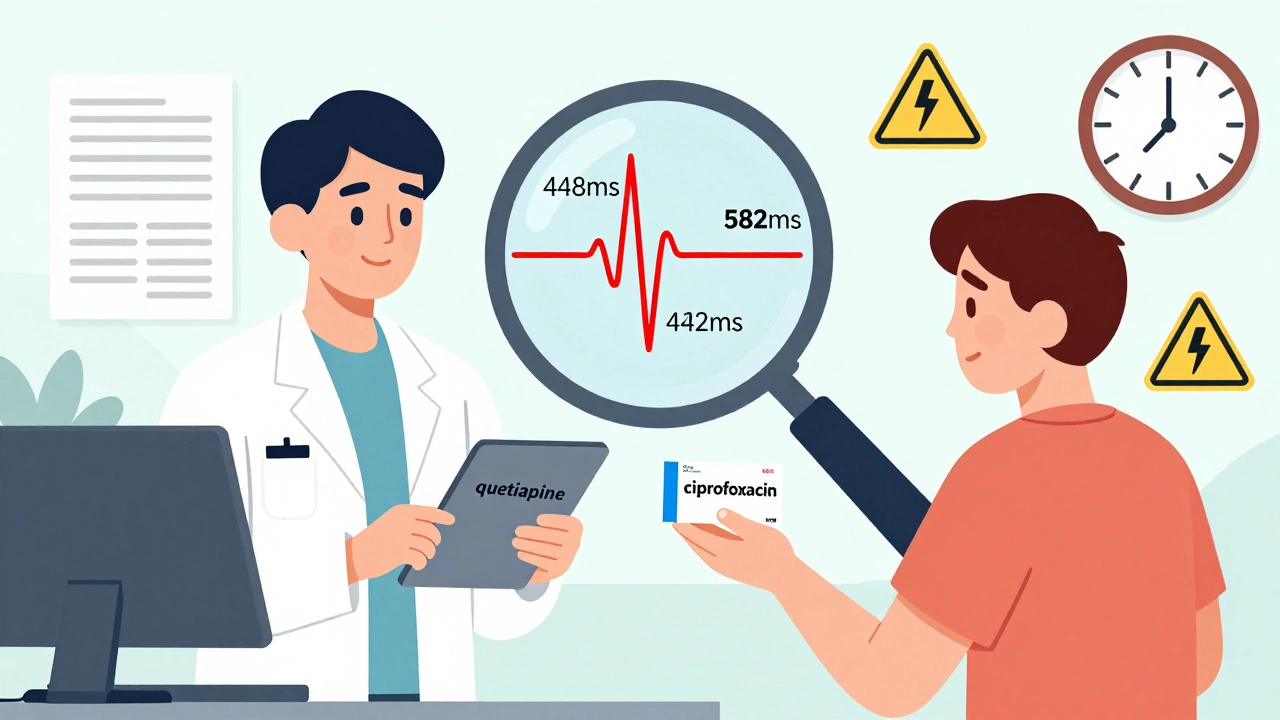
Your heart beats because of electrical signals. The QT interval on an ECG measures how long it takes for your heart’s lower chambers to recharge between beats. If that interval gets too long, your heart can slip into a dangerous rhythm called torsades de pointes. It’s rare, but when it happens, it can lead to sudden cardiac arrest. Normal QTc (corrected QT) is under 440 ms for men and 460 ms for women. Once it hits 500 ms or higher, your risk of a life-threatening arrhythmia jumps fivefold.Which Antipsychotics Are Riskiest?
Not all antipsychotics are created equal when it comes to heart risk. Some are much more likely to block the hERG potassium channel, which controls repolarization. Thioridazine, once widely used, was pulled from the U.S. market in 2005 because it caused so many cardiac deaths. It’s still prescribed in some countries and remains one of the most dangerous-7.8 times higher risk of sudden death compared to non-users. Today’s high-risk options include ziprasidone and haloperidol. Both have strong hERG blockade, with IC50 values below 0.2 μM. Moderate-risk drugs like quetiapine, risperidone, and olanzapine are far more common. In fact, quetiapine alone accounts for over 24 million prescriptions a year in the U.S. Despite the known risks, these are still first-line choices because they’re effective and better tolerated than older drugs. On the safer end: aripiprazole, brexpiprazole, and lurasidone. Their hERG blockade is weak-IC50 values above 10 μM-and studies show they don’t significantly increase sudden death risk. Aripiprazole’s risk is nearly the same as not taking any antipsychotic at all.It’s Not Just the Antipsychotic-It’s What You Mix It With
The real danger comes from combinations. Almost half of people on antipsychotics are also taking another drug that prolongs QT. Common culprits include:- Antibiotics: moxifloxacin, ciprofloxacin
- Antiemetics: ondansetron, domperidone
- Antiarrhythmics: sotalol, amiodarone
- Antidepressants: citalopram, escitalopram
Who’s Most at Risk?
It’s not just about the drugs. Your body matters too. Certain factors stack the deck:- Age over 65: adds 15.3 ms to QTc
- Female sex: adds 12.8 ms
- Low potassium (below 3.5 mmol/L): adds 22.7 ms
- Low magnesium: worsens the effect
- Heart disease or bradycardia (heart rate under 50): adds 18.4 ms
- Genetic factors: Poor metabolizers of CYP2D6 (7-10% of Caucasians) build up drug levels faster
What Should You Do? A Practical Guide
If you’re on an antipsychotic-or considering one-here’s what actually works:- Get a baseline ECG before starting. Don’t wait for symptoms. Do it before the first dose.
- Know your drug combo. Ask your doctor or pharmacist: ‘Is this drug on the QT-prolonging list?’ Use resources like www.crediblemeds.org to check.
- Monitor potassium and magnesium. Low levels are a silent trigger. Blood tests every 2-4 weeks in high-risk cases can prevent 82% of torsades cases.
- Follow-up ECGs matter. For high-risk combinations, get an ECG weekly for the first month, then monthly. For moderate risk, check at 1 week, 4 weeks, then quarterly.
- Watch for warning signs. Dizziness, fainting, palpitations, or sudden fatigue aren’t ‘just stress.’ They could be your heart warning you.

Why Aren’t More People Getting Checked?
The guidelines are clear. But reality is messy. Only 35% of community clinics regularly monitor QTc, even though the American Heart Association says they should. Why?- Insurance denies ECGs unless you’re hospitalized.
- Rural clinics don’t have ECG machines.
- Doctors don’t have time to interpret them.
- Patients are scared-29% quit their meds because they fear heart problems.
Ada Maklagina
December 6, 2025 AT 12:23My grandma was on quetiapine and got cipro for a UTI. She collapsed at the grocery store. No one knew why until the ER did an ECG. Scary as hell. They switched her to aripiprazole and she’s been fine since. Just sayin’.
Norene Fulwiler
December 7, 2025 AT 08:07I’m a nurse in a psych unit. We’ve had two code blues in the last year from QT prolongation. One was a 22-year-old on ziprasidone + ondansetron. They didn’t even know the antibiotic was a problem. We now do ECGs on Day 1. No excuses. Lives are on the line.
William Chin
December 8, 2025 AT 16:17It is imperative that clinicians adhere to evidence-based protocols regarding cardiac monitoring in patients prescribed antipsychotic medications. The American Heart Association has unequivocally delineated the necessity of baseline and serial electrocardiographic assessments. Failure to comply constitutes a breach of the standard of care, and may constitute negligence under tort law. Furthermore, the financial burden of adverse cardiac events far exceeds the cost of routine ECGs.
Harry Nguyen
December 9, 2025 AT 16:31Oh wow, another ‘drug is dangerous’ article. Next you’ll tell me water can kill you if you drink too much. People die from falling down stairs too. Should we ban stairs? Also, why are we letting foreigners prescribe meds? This country’s healthcare is a joke.
Katie Allan
December 9, 2025 AT 21:19This is exactly the kind of information that needs to be in every patient’s hands-not buried in medical journals. I’ve seen too many people stop their meds out of fear, not because they were informed. Knowledge isn’t fear-it’s power. If you’re on an antipsychotic, print this out. Bring it to your doctor. Ask the questions. You deserve to live, not just survive.
Deborah Jacobs
December 11, 2025 AT 07:46Man, I remember when my cousin was on risperidone and got prescribed Z-Pak for a sinus infection. She started feeling like her heart was trying to escape her chest. She thought she was having a panic attack-turns out her QTc was 520. They rushed her in. She cried for a week after, not because she was scared of dying, but because she felt so damn stupid for not asking. Don’t be like her. Ask. Even if you think you sound dumb. Your heart doesn’t care how smart you are.
James Moore
December 12, 2025 AT 07:30Let’s be honest-this whole QT prolongation thing is just another example of the pharmaceutical-industrial complex weaponizing fear to push their ‘safer’ alternatives. Aripiprazole? It’s still a dopamine modulator. It’s still altering brain chemistry. And yet, suddenly it’s the ‘gold standard’? What about the fact that these drugs are prescribed to children? To the elderly? To people with no family support? The system isn’t broken-it’s designed this way. We’re being manipulated into thinking we can ‘optimize’ our minds with pills while ignoring the root causes: poverty, trauma, isolation. The ECG is a band-aid on a bullet wound.
Manish Shankar
December 13, 2025 AT 00:15As a physician in rural India, I can confirm that access to ECG monitoring remains a critical challenge. Many patients cannot afford even basic cardiac screening. However, the principles outlined in this article are universally applicable. We have started educating our patients using simple visual charts and local language pamphlets. The risk is real, but awareness-even at a basic level-can prevent tragedy. Thank you for highlighting this issue.
luke newton
December 14, 2025 AT 09:33Why do people on antipsychotics always think they’re special? You’re not the first person to have a heart issue. Everyone’s heart can be messed up by something. Maybe you should’ve thought twice before taking a mind-altering drug in the first place. Stop blaming doctors. Stop blaming drugs. Take responsibility.
Ali Bradshaw
December 15, 2025 AT 06:23Just wanted to say-this post saved my life. I was on olanzapine + citalopram. My QTc was creeping up. I didn’t know until I read this. I switched to lurasidone. My ECG’s normal now. I’m not just stable-I’m alive. Thank you for writing this. You’re not just a doctor. You’re a lifeline.
an mo
December 15, 2025 AT 19:54Per the FDA Adverse Event Reporting System (FAERS), the relative risk of torsades de pointes for high-potency hERG blockers like ziprasidone in polypharmacy cohorts demonstrates a 4.7-fold increase (95% CI: 3.9–5.5) with concomitant CYP3A4 inhibitors. Furthermore, the population attributable fraction for QTc prolongation-related mortality in psychiatric populations exceeds 12% annually. The economic burden of preventable arrhythmias in Medicare beneficiaries alone exceeds $470M/year, primarily due to prolonged hospitalization and ICU admission. Regulatory compliance is not optional-it’s actuarially inevitable.