Bursitis and Tendinitis: How to Tell Them Apart and Treat Them Right
 Jan, 12 2026
Jan, 12 2026
When your shoulder aches after lifting boxes, or your knee hurts when you kneel down, it’s easy to assume it’s just "overuse." But not all joint pain is the same. Two very common conditions - bursitis and tendinitis - often get mixed up, even by doctors. Yet treating them the same way can make things worse. Understanding the difference isn’t just academic - it changes how you recover.
What Exactly Is Bursitis?
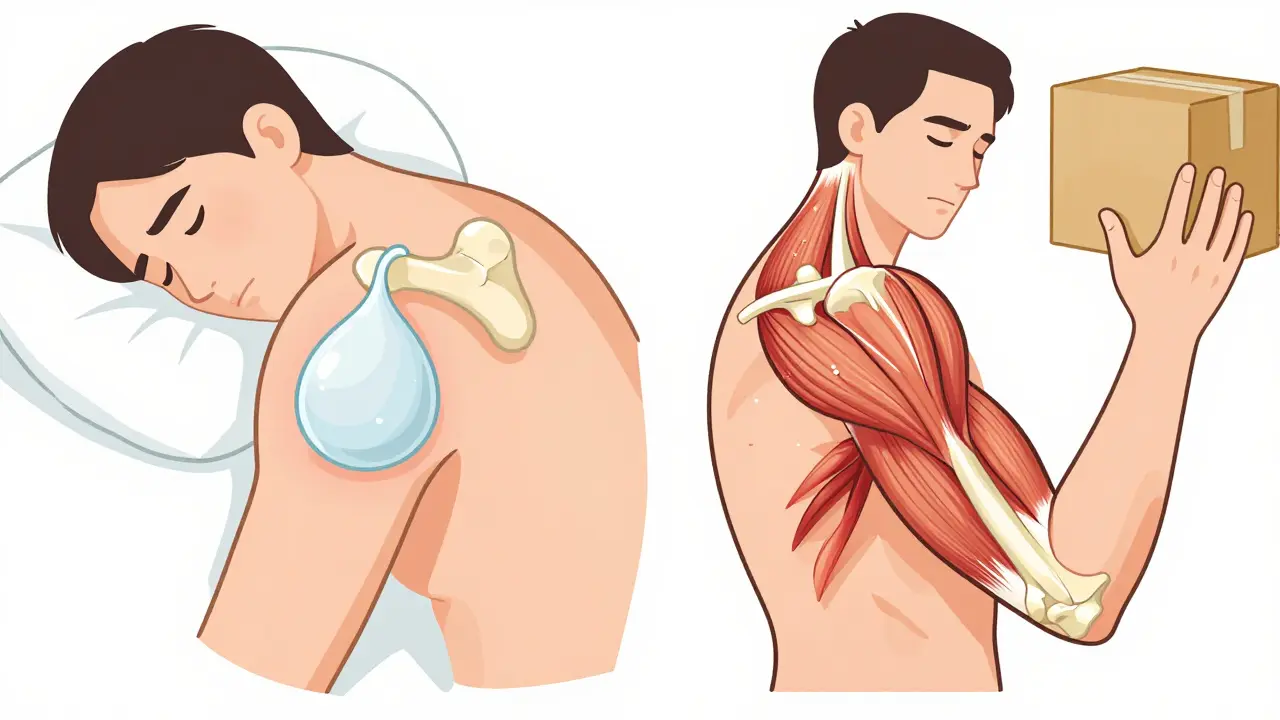
Bursitis happens when a bursa - a tiny, fluid-filled sac that acts like a cushion between bones and tendons - gets inflamed. There are about 160 of these sacs in your body, but only a few commonly cause trouble. The most frequent spots are the shoulder (subacromial), elbow (olecranon), hip (trochanteric), and knee (prepatellar).
Think of a bursa like a water balloon between your bones and skin. When it swells up from too much friction or pressure, it pushes on nerves and causes pain. You might feel a dull, achy pain around the joint, especially when you lie on it at night. Swelling might be visible - like a soft lump on the elbow or knee. The pain doesn’t always follow a specific movement pattern. It just... hurts when you move or press on it.
Common triggers? Kneeling for hours (carpet layers, gardeners), leaning on your elbows (desk workers), or repetitive overhead motions (painters, swimmers). It’s more common after 40, and women over 50 are slightly more likely to get hip bursitis than men.
What Exactly Is Tendinitis?
Tendinitis is inflammation of a tendon - the tough, fibrous tissue that connects muscle to bone. Unlike bursae, tendons don’t cushion. They pull. When they’re overworked, tiny tears form, and the body responds with inflammation. The most common tendons affected are the rotator cuff (shoulder), Achilles (ankle), patellar (knee), and wrist extensors (tennis elbow).
The pain from tendinitis is different. It doesn’t just ache - it pulls. You’ll feel sharp pain along the tendon’s path during specific movements. Try bending your wrist? Pain on the outside of your elbow. Jumping? Pain under your kneecap. Rising from a chair? Pain in your hip or thigh. It’s movement-specific. And unlike bursitis, the pain often gets worse with activity, not better.
Here’s a key point: many chronic cases aren’t truly "inflammatory" anymore. Experts now call them tendinopathy - degeneration without active swelling. That’s why rest alone often fails. You need to rebuild the tendon, not just calm it down.
How Do You Know Which One You Have?
Doctors don’t guess. They test. Here’s what they look for:
- Bursitis: Pain is diffuse - spread out over the joint. Tenderness is focused on the bursa’s location. Swelling may be visible. Pain worsens when you lie on the area. No sharp pain during specific movements - just constant pressure.
- Tendinitis: Pain follows the line of the tendon. You’ll feel it when you stretch or contract the muscle attached to it. Try the "resisted movement" test: if moving against resistance hurts, it’s likely the tendon.
And here’s the kicker: they often happen together. In fact, 65% of shoulder pain cases involve both rotator cuff tendinitis and subacromial bursitis. That’s why misdiagnosis is so common. If you’re told you have "shoulder tendonitis" but your pain is worse when you lie on your side - you might actually have bursitis.
Ultrasound is the best tool to tell them apart. It shows fluid buildup in bursae and thickening or tears in tendons. MRI is more detailed but often unnecessary unless symptoms last more than 6 weeks.

What Treatments Actually Work?
Forget the old advice: "Rest and ice." That’s only step one. Here’s what works - based on real outcomes from thousands of patients.
For Bursitis
Most cases improve in 4-6 weeks with simple steps:
- Stop the pressure. If it’s your elbow, don’t lean on it. If it’s your hip, avoid crossing your legs or sleeping on that side.
- Cold therapy. Ice packs for 15 minutes, 3-4 times a day. Frozen water bottles rolled over the area work better than ice cubes - they conform to the shape.
- NSAIDs. Ibuprofen or naproxen for 7-10 days max. Longer increases stomach bleeding risk.
- Corticosteroid injection. If pain doesn’t improve in 2 weeks, an injection into the bursa has a 78% success rate at 4 weeks. It’s fast, effective, and safe when done under ultrasound guidance.
Don’t inject into tendons. That’s a big mistake. Steroids can weaken tendons and cause rupture. That’s why knowing the difference matters.
For Tendinitis
Tendinitis needs more than rest. You need to rebuild.
- Stop aggravating movements. No heavy lifting, no jumping, no repetitive motions - but don’t stop moving entirely.
- Eccentric strengthening. This is the gold standard. For Achilles tendinitis: stand on a step, rise on both feet, then lower slowly on just the injured foot. Do 3 sets of 15 reps, twice daily, for 12 weeks. For shoulder: use a resistance band to slowly lower your arm after lifting it. This rebuilds tendon strength better than any injection.
- Corticosteroid injections? Only if pain is severe and persistent. Success rate? Only 52% at 4 weeks. And the relief doesn’t last. In fact, 34% of tendinitis patients report temporary worsening after injection.
- Platelet-rich plasma (PRP). For chronic cases that don’t respond, PRP - a shot of your own concentrated blood platelets - has shown 67% improvement at 6 months, compared to 42% with steroids. Cost? Around $850 per shot. But for athletes or people who can’t afford long-term pain, it’s worth considering.
What to Avoid
Many people make the same mistakes - and it delays recovery.
- Doing stretches too early. Stretching an inflamed tendon or bursa makes it worse. Wait until pain drops below 3/10 before stretching.
- Ignoring pain levels. If exercise hurts more than 3/10, you’re pushing too hard. The "pain monitoring rule" - staying under 3/10 during rehab - is backed by physical therapists and research.
- Over-relying on imaging. A 2022 study found 40% of people over 50 have bursitis or tendinitis on MRI - but no symptoms. Don’t treat a scan. Treat the person.
- Taking opioids. The CDC says opioids should never be first-line for these conditions. Yet 12.7% of patients still get them. That’s dangerous and unnecessary.
Real People, Real Recovery
On Reddit’s r/PhysicalTherapy, users share what actually helped:
- One man with chronic Achilles tendinitis did 180 eccentric heel drops a day for 27 weeks. He tracked progress with the VISA-A questionnaire - his score jumped from 42 to 89.
- A woman with hip bursitis switched from sleeping on her side to a body pillow between her legs. Her pain dropped 80% in 3 weeks.
- A construction worker with knee bursitis started using knee pads. He cut his flare-ups by 90%.
And the most common tip? Ice rolling. Freeze a water bottle, roll it under your knee or along your Achilles for 10 minutes. It’s cheap, effective, and easy to do at home.

When to See a Doctor
You don’t need to wait until you’re crippled. See a provider if:
- Pain lasts more than 2 weeks despite rest and ice
- You can’t move the joint without severe pain
- You notice weakness or numbness
- Swelling, redness, or fever develops - this could mean infection
Physical therapists are your best allies. Certified hand therapists (available at most major hospitals) specialize in upper-body issues. For Achilles or knee problems, look for therapists trained in Alfredson’s eccentric protocol.
Prevention Is Easier Than Cure
These conditions don’t come out of nowhere. They build over time.
- Warm up. Five minutes of light cardio before activity - even walking - increases blood flow to tendons and bursae.
- Strengthen. Weak muscles put more stress on tendons. Do regular resistance training - not just when you’re in pain.
- Modify your workspace. If you type all day, raise your keyboard so your wrists are neutral. If you kneel, use a cushion.
- Listen to your body. If a movement hurts consistently, change it. Don’t push through.
Wearable tech like the Apple Watch is starting to help. Its motion sensors can detect abnormal movement patterns linked to tendinitis risk - before you even feel pain. Early detection means prevention.
Bottom Line
Bursitis and tendinitis aren’t the same. One is about cushioning, the other about pulling. One responds to rest and injections. The other needs rebuilding. Misdiagnose one for the other, and you could be setting yourself up for months of unnecessary pain - or even a tendon rupture.
Start with the basics: stop what hurts, ice it, take NSAIDs for a week. If it doesn’t improve, get an ultrasound. Don’t assume. Don’t guess. Know what you’re treating - and treat it right.
Angel Tiestos lopez
January 12, 2026 AT 16:15also tbh i think bursitis is just the body’s way of saying ‘hey u suck at posture’ 😅
Trevor Davis
January 12, 2026 AT 22:18And yes - eccentric training is the real MVP. I did 12 weeks of heel drops for Achilles tendinopathy. It felt like torture. Now I run 5Ks again. Worth every sob.
mike swinchoski
January 13, 2026 AT 09:45Damario Brown
January 13, 2026 AT 22:29and why is PRP $850? because insurance won’t cover it and clinics are milking the wellness-industrial complex. same with ‘vibration plates’ and ‘red light therapy’ - all placebo with a price tag.
sam abas
January 14, 2026 AT 08:54why do we need to label it? why not just say ‘stop doing the thing that hurts’ and then slowly reintroduce movement? why the jargon? why the ultrasound? why the PRP? why not just… move better?
also, the apple watch thing? cute. my watch tells me i didn’t walk enough. it doesn’t tell me why my shoulder feels like it’s full of wet sand.
and can we talk about how 40% of people over 50 have ‘asymptomatic bursitis’ on MRI? that means half the people reading this are probably being told they have something they don’t even feel. we’re pathologizing aging. again.
John Pope
January 14, 2026 AT 21:06but let me ask you this - if tendons are degenerating, why are we treating them like they’re broken phones? ‘Oh, your tendon’s frayed? Here’s a patch job with your own blood.’
what if the problem isn’t the tendon? what if it’s your entire movement pattern? your breathing? your stress? your sleep? your trauma? your soul?
you’re all so focused on the tissue you’ve forgotten the human.
also - i did 180 heel drops. i cried. i screamed. i felt enlightened. now i’m a ‘tendon whisperer’.
you’re welcome.
Clay .Haeber
January 16, 2026 AT 10:44and the real MVP is a guy who did 180 heel drops for 27 weeks? wow. what a revolutionary breakthrough. next you’ll tell me the cure for cancer is drinking lemon water while reciting the constitution.
also, ‘don’t inject steroids into tendons’? thanks for the tip, Dr. Obvious. I’m sure every MD in the world just woke up from a 50-year coma hearing that.
and PRP at $850? congrats, you’ve turned human biology into a luxury spa package. I’ll take the placebo, please. With extra glitter.
Priyanka Kumari
January 16, 2026 AT 12:43Also, the ice bottle trick? Yes. It’s simple, it’s cheap, and it works. I teach it to my patients every day.
One thing I’d add: don’t underestimate the power of sleep and hydration. Tendons and bursae heal best when your whole body is supported. You can’t out-train poor recovery.
And please - if you’re in pain, don’t wait until it’s crippling. Early movement, guided by a pro, makes all the difference.