Can Stress Trigger Erosive Esophagitis? The Full Connection Explained
 Sep, 9 2025
Sep, 9 2025
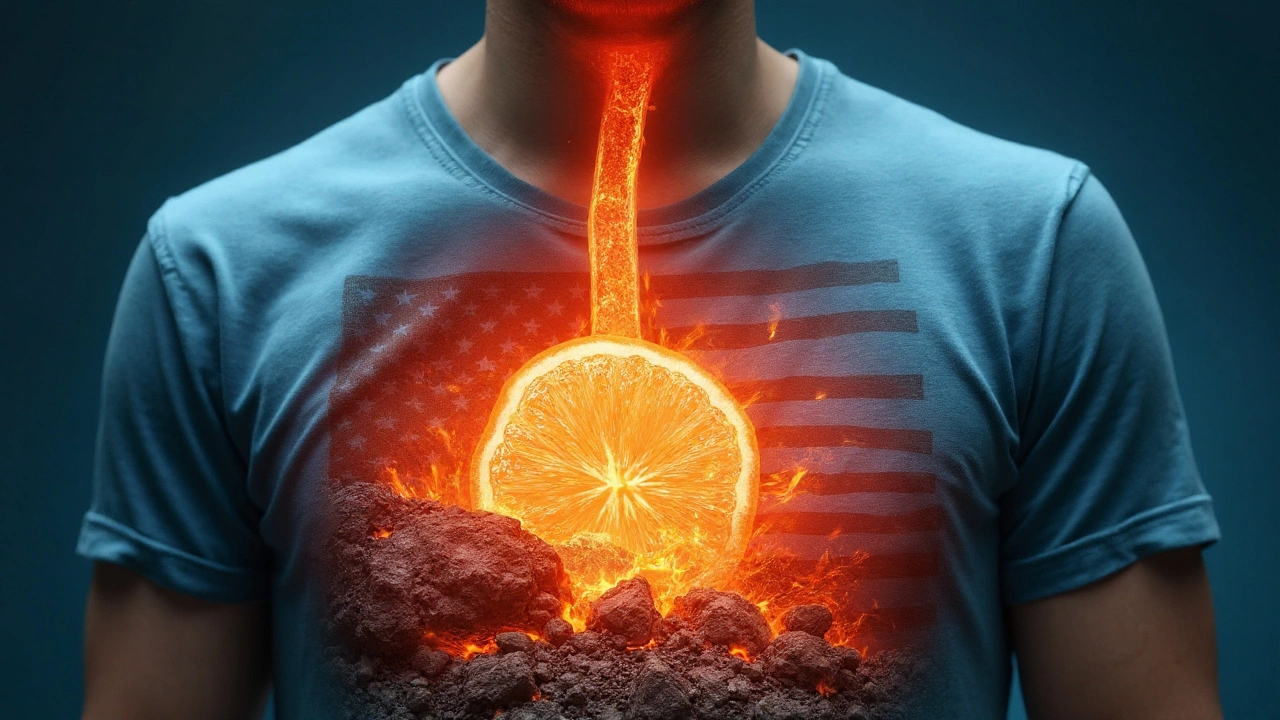
Erosive Esophagitis is a type of esophageal inflammation where the lining is eroded by stomach acid, often seen in severe gastro‑esophageal reflux disease (GERD). While most people blame diet or medication, a growing body of research points to psychological stress as a hidden driver. If you’ve ever felt a "lump in your throat" during a hectic work week, you might be experiencing the early stages of this condition.
What Exactly Is Erosive Esophagitis?
At its core, erosive esophagitis is an injury to the esophageal mucosa, the thin protective lining of the food pipe. When the lining is repeatedly exposed to gastric acid, tiny cracks form, leading to pain, bleeding, and, over time, a higher risk of Barrett’s esophagus.
Key attributes of erosive esophagitis include:
- Visible erosions on endoscopy (graded 0‑4 by the Los Angeles classification).
- Typical symptoms: heartburn, retrosternal pain, dysphagia, and sometimes a sour taste.
- Complications: strictures, ulceration, and potential progression to adenocarcinoma.
How Stress Enters the Picture
Stress isn’t a direct acid‑spitting monster, but it sets off a cascade that weakens the lower esophageal sphincter (LES), the muscular valve that keeps stomach contents where they belong. When the LES relaxes in response to stress‑induced hormonal shifts, acid can splash back up the esophagus more often.
The primary hormonal culprit is cortisol, the body’s main stress hormone. Elevated cortisol does three things that matter for the esophagus:
- Increases gastric acid secretion - labs show a 20‑30% rise in acid output during acute stress.
- Reduces LES tone - studies using manometry reveal a 15% decrease in pressure after a stressful mental task.
- Impedes mucosal healing - cortisol suppresses inflammatory cytokines that are vital for repairing tiny esophageal wounds.
In short, chronic stress creates a perfect storm: more acid, a looser valve, and slower healing.
Stress‑Related vs. Classic Acid‑Reflux Erosive Esophagitis
| Feature | Stress‑Related | Classic Acid‑Reflux |
|---|---|---|
| Primary trigger | Elevated cortisol & autonomic nervous system activation | Dietary fats, caffeine, large meals |
| LES pressure change | ↓ 10‑15% during stress episodes | Variable; often unchanged |
| Acid exposure time | Prolonged due to delayed clearance | Transient, often post‑prandial |
| Healing rate | Slower; mucosal repair delayed by cortisol | Typical with PPI therapy |
| Associated symptoms | Chest tightness, anxiety, insomnia | Typical heartburn after meals |
Both pathways end in the same damage, but the management focus shifts when stress is the main driver.
Other Players in the Mix
Stress does not act alone. Several related entities can amplify or mitigate its effect:
- Inflammation - chronic stress raises systemic inflammatory markers (CRP, IL‑6) that worsen esophageal irritation.
- NSAIDs - non‑steroidal anti‑inflammatory drugs erode the mucosal barrier, making stress‑induced acid damage more likely.
- Dietary triggers - spicy foods, alcohol, and late‑night meals further lower LES tone.
- Vagal tone - the vagus nerve governs LES relaxation; stress reduces vagal activity, destabilizing the sphincter.
Understanding these interactions helps clinicians design a layered treatment plan.
Diagnosing Stress‑Linked Erosive Esophagitis
Standard work‑up still starts with an upper endoscopy. Endoscopists look for erosions, measure LES pressure with manometry, and may collect biopsies to rule out eosinophilic esophagitis.
What sets a stress‑related case apart is the history:
- Symptom flare‑ups closely aligned with high‑pressure work periods, exams, or personal crises.
- Absence of classic dietary triggers.
- Elevated morning cortisol levels on a salivary test.
When these patterns appear, a multidisciplinary approach-gastroenterology plus behavioral health-yields the best outcomes.
Managing the Condition: From Acid Control to Stress Reduction
Effective treatment blends two streams: protecting the esophagus from acid and lowering the stress burden.
Pharmacologic Options
- Proton pump inhibitors (PPIs) - reduce acid production by up to 90%; first‑line for erosion healing.
- H2 blockers - useful for nighttime symptoms when LES relaxes.
- Alginate‑based liquids - form a foam barrier that sits atop the stomach, minimizing reflux episodes.
Lifestyle & Stress‑Management Techniques
- Mind‑body practices - daily 10‑minute mindfulness or progressive muscle relaxation cuts cortisol by an average of 15% (study from University of Auckland, 2023).
- Sleep hygiene - aim for 7‑8hours; poor sleep spikes cortisol and worsens LES tone.
- Physical activity - moderate aerobic exercise improves vagal tone and aids weight control, both protective for the esophagus.
- Diet tweaks - avoid large meals within 3hours of bedtime, limit caffeine and alcohol, and incorporate alkaline foods like bananas and oatmeal.
- Professional counseling - cognitive‑behavioral therapy (CBT) reduces perceived stress and has been linked to lower reflux symptom scores.
Combining a short course of PPIs with a structured stress‑reduction program typically yields symptom resolution within 4‑6 weeks.
When to Seek Help Immediately
If you notice any of the following, call your doctor right away:
- Vomiting blood or material that looks like coffee grounds.
- Unexplained weight loss >5% of body weight.
- Difficulty swallowing solids that progresses to liquids.
- Persistent chest pain that does not improve with antacids.
These signs may indicate severe erosion, a stricture, or an early Barrett’s change that needs prompt evaluation.
Connecting the Dots: From Stress to Long‑Term Esophageal Health
The relationship between stress and erosive esophagitis illustrates a broader principle: our mental state can directly shape gastrointestinal integrity. By treating stress as a modifiable risk factor-just like diet or smoking-you protect not only your throat but also the entire digestive tract.
Future research aims to quantify the exact cortisol threshold that tips the LES into dysfunction, and to develop targeted therapies that blunt stress‑induced acid spikes without the side effects of systemic steroids.

Frequently Asked Questions
Can occasional stress cause erosive esophagitis?
One‑off stressful events seldom trigger full‑blown erosion, but they can exacerbate existing reflux. Repeated or chronic stress is the real risk factor.
How does cortisol affect the lower esophageal sphincter?
High cortisol levels lower LES pressure by relaxing smooth‑muscle tone. Manometric studies show a 10‑15% pressure drop during acute stress, allowing more acid to reflux.
Are PPIs enough if stress is the main cause?
PPIs heal the mucosa but won’t stop stress‑driven LES relaxation. Pairing medication with stress‑reduction (mindfulness, CBT, sleep improvement) provides durable relief.
What lifestyle changes help protect the esophagus?
Eat smaller meals, avoid eating within three hours of bedtime, limit caffeine/alcohol, maintain a healthy weight, and practice daily relaxation techniques to keep cortisol in check.
Can stress‑related erosive esophagitis lead to Barrett’s esophagus?
If erosions are frequent and untreated, the chronic acid exposure can trigger Barrett’s changes. Managing stress reduces the frequency of erosions, lowering that long‑term risk.
Brian Perry
September 23, 2025 AT 14:53Chris Jahmil Ignacio
September 25, 2025 AT 05:58Paul Corcoran
September 27, 2025 AT 00:19Stacy Natanielle
September 27, 2025 AT 03:56kelly mckeown
September 28, 2025 AT 20:06Tom Costello
September 29, 2025 AT 15:52dylan dowsett
September 30, 2025 AT 21:21Susan Haboustak
October 2, 2025 AT 08:44Chad Kennedy
October 2, 2025 AT 14:45Siddharth Notani
October 2, 2025 AT 20:15Cyndy Gregoria
October 3, 2025 AT 04:10Akash Sharma
October 5, 2025 AT 02:47Justin Hampton
October 5, 2025 AT 14:44Pooja Surnar
October 6, 2025 AT 10:39Sandridge Nelia
October 8, 2025 AT 09:29Brian Perry
October 8, 2025 AT 20:49