CBD Oil Interactions with Prescription Drugs: CYP450 Inhibition & Sedation Risks
 Oct, 26 2025
Oct, 26 2025
CBD Drug Interaction Checker
Check Your Medication Interactions
CBD inhibits several liver enzymes (CYP450), which can affect how your medications work. Enter your prescription drugs to see potential interactions.
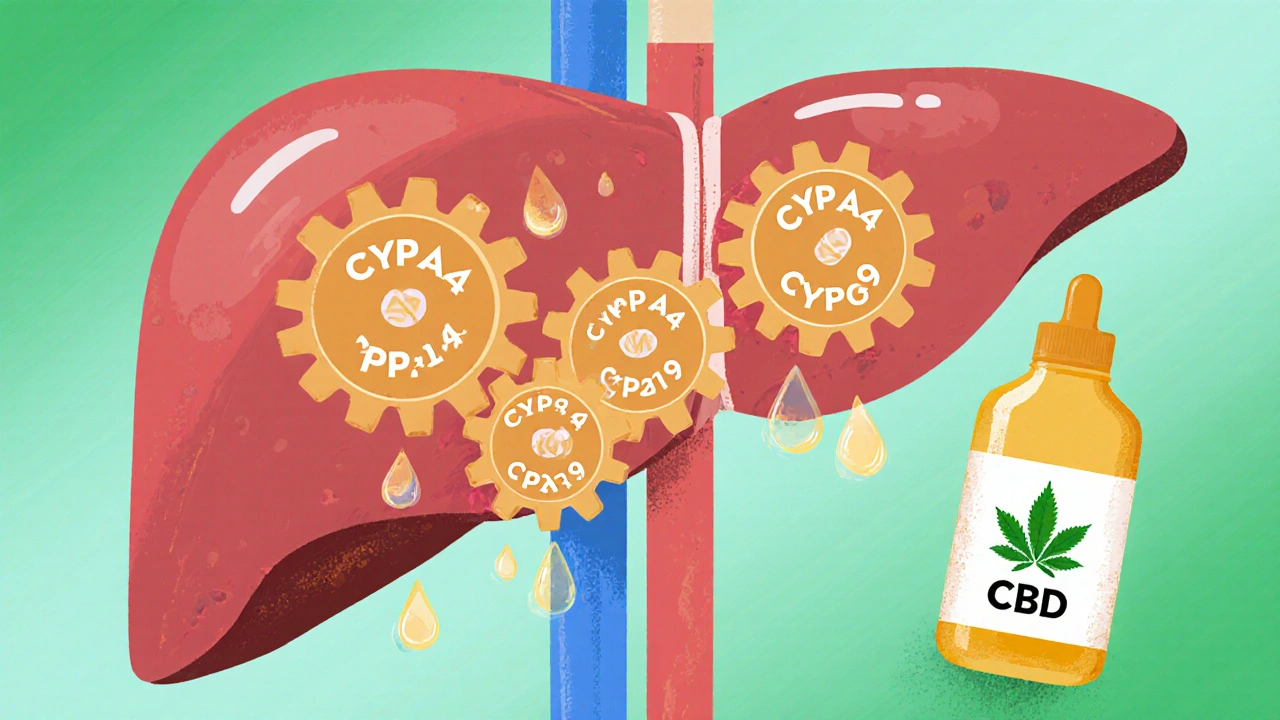
CBD Oil is a cannabinoid extract from Cannabis sativa that many people take for wellness or medical reasons; it can inhibit cytochrome P450 enzymes in the liver. When you mix it with prescription meds, the result can be unexpected side‑effects, altered drug levels, and sometimes dangerous sedation. This guide walks through how the enzyme system works, which drugs are most vulnerable, real‑world stories, and practical steps you can take to stay safe.
Key Takeaways
- CBD strongly inhibits several CYP450 isoforms, especially CYP3A4, CYP2C19, and CYP2C9.
- Medications metabolized by those enzymes - such as Warfarin (an anticoagulant with a narrow therapeutic index and Clobazam (a benzodiazepine used for seizures) - can see dramatic level spikes when taken with CBD.
- Increased drug levels often translate into heightened sedation, bleeding risk, or other serious effects.
- Therapeutic drug monitoring, dose adjustments, and timing tweaks manage most interactions effectively.
- Emerging formulations aim to retain CBD’s benefits while lowering CYP inhibition.
How CBD Targets the CYP450 Enzyme Family
The liver’s cytochrome P450 system handles roughly 75% of all prescription drug metabolism. Key isoforms include CYP1A2, CYP2B6, CYP2C9, CYP2C19, CYP2D6, CYP2E1, and CYP3A4. Research from Yamaori et al. (2010‑2012) showed that cannabidiol (CBD) acts as a reversible inhibitor across most of these enzymes.
CBD’s potency varies by isoform. The most recent comprehensive study (PMID 11022895) reported IC50 values ranging from 0.03 µM (CYP2B6) to about 1 µM (CYP1A2). At therapeutic plasma concentrations of 1‑2 µM, CBD meaningfully blocks CYP2C9, CYP2C19, and CYP3A4 - the enzymes that process roughly half of all prescription drugs.
Why does this matter? When CBD slows an enzyme, the drug that normally relies on that pathway hangs around longer in the bloodstream. Higher concentrations mean stronger effects, and, for narrow‑therapeutic‑index meds, that can be dangerous.
Prescription Medications Most at Risk
Not every drug is equally vulnerable. The biggest red flags are drugs that are primarily cleared by the isoforms CBD inhibits the most.
- Warfarin - metabolized by CYP2C9. CBD can raise INR values, leading to bleeding.
- Clobazam - relies on CYP2C19. CBD raises its active metabolite N‑desmethyl‑clobazam up to 60%, causing excessive sedation.
- Selective serotonin reuptake inhibitors (SSRIs) such as fluoxetine and paroxetine - CYP2D6 substrates; CBD can increase plasma levels and side‑effects.
- Calcium‑channel blockers like amlodipine - CYP3A4 clearance; CBD may boost blood pressure‑lowering effects.
- Opioids (e.g., fentanyl, oxycodone) - CYP3A4 metabolism; combined use can deepen sedation.
- Statins such as simvastatin - CYP3A4; risk of muscle toxicity rises.
These examples cover roughly 70% of all high‑risk interactions reported in the FDA’s Adverse Event Reporting System between 2018‑2023.
When Sedation Turns Dangerous
CBD‑induced enzyme inhibition often shows up as deeper, longer‑lasting sedation. Real‑world cases illustrate the problem.
On Reddit’s r/Epilepsy community, a user shared that after starting Epidiolex (a prescription CBD formulation approved for certain seizure disorders at 5 mg/kg/day, their clobazam level jumped from 600 ng/mL to 1,050 ng/mL within two weeks, causing extreme drowsiness. Their neurologist cut the clobazam dose by half.
Another patient posted on PatientsLikeMe that taking over‑the‑counter CBD oil with warfarin pushed their INR from 2.5 to 5.8 in ten days, triggering an emergency vitamin K infusion.
These anecdotes match the FAERS data: 147 sedation‑related reports linked to CBD, with 32% involving antiepileptic drugs and 28% tied to benzodiazepines.
Managing the Interaction: Practical Strategies
Clinicians and patients can take concrete steps to reduce risk.
- Start Low, Go Slow. The FDA label for Epidiolex recommends beginning at 2.5 mg/kg twice daily, then titrating up while monitoring co‑meds.
- Therapeutic Drug Monitoring (TDM). For narrow‑index drugs like warfarin or certain antiepileptics, check blood levels 3‑5 days after introducing CBD and adjust doses accordingly.
- Pre‑emptive Dose Reduction. For known CYP2C19 substrates (e.g., clobazam), reduce the prescription dose by 25‑50% when starting CBD.
- Stagger Dosing Times. Separate CBD and the interacting medication by 2‑4 hours to lower peak overlap.
- Alternative Cannabinoids. Minor cannabinoids such as CBG show far less CYP inhibition; they may be a safer option when the therapeutic goal is inflammation or pain without drug‑interaction worries.
- Pharmacist Involvement. ASHP 2022 guidelines advise pharmacists to flag any CBD‑prescription combo involving CYP2C9, CYP2C19, or CYP2D6.
When dose adjustment isn’t enough, clinicians may switch the patient to a non‑CYP‑dependent drug or temporarily pause CBD.

Clinical Guidelines and Educational Resources
Several professional bodies have codified best practices.
- American Society of Health‑System Pharmacists (ASHP, 2022) - recommends avoiding concurrent CBD with narrow‑therapeutic‑index drugs metabolized by CYP2C9, CYP2C19, or CYP2D6.
- FDA Epidiolex Prescribing Information - mandates dose reductions for CYP2C19 substrates and regular INR checks for warfarin.
- University of Maryland CME Course - “Cannabis‑Drug Interactions: Clinical Management,” taken by over 1,200 clinicians in 2023.
- University of Washington Cannabis‑Drug Interaction Checker - beta‑released June 2024; a free online tool that flags high‑risk combos.
Staying current with these resources helps clinicians anticipate problems before they happen.
Future Outlook: Research and Market Trends
The interaction landscape is evolving fast. The global CBD market hit $28.6 billion in 2023, and with 45% of users taking a prescription drug alongside CBD, the demand for interaction testing is soaring. The interaction‑testing market is projected to reach $489 million by 2028 (CAGR 30.7%).
Key research pipelines include:
- NIH‑funded warfarin probe study (NCT04893224) - measuring CBD’s effect on CYP2C9 activity in 120 volunteers; first results expected Q3 2024.
- Axim Biotechnologies nanoparticle CBD - aims to limit hepatic exposure, potentially reducing CYP inhibition; Phase I data due Q4 2024.
- European Medicines Agency (EMA) 2024 guideline - now requires every cannabinoid‑based medicine to list CYP450 interaction data on the label.
These advances suggest that while CBD’s enzyme inhibition remains a challenge, smarter formulations and better decision‑support tools will make co‑prescribing safer.
Quick Checklist for Patients and Providers
- Identify all prescription meds, especially those cleared by CYP3A4, CYP2C19, CYP2C9, or CYP2D6.
- Ask the prescriber if a dose reduction is needed before starting CBD.
- Schedule baseline blood‑level tests (INR, drug trough levels) before adding CBD.
- Re‑check levels after 3‑5 days of CBD initiation.
- Monitor for signs of excess sedation, bleeding, or cardiac changes.
- Document the timing of each dose to help interpret blood‑test results.
Conclusion
While CBD oil interactions can be scary, they’re manageable with the right knowledge. Knowing which enzymes CBD blocks, recognizing the drugs most at risk, and following evidence‑based monitoring protocols lets you enjoy CBD’s potential benefits without compromising safety. Keep an eye on emerging research-new formulations may soon give us the best of both worlds.

What is the main way CBD interacts with prescription drugs?
CBD inhibits several cytochrome P450 enzymes in the liver-especially CYP3A4, CYP2C19, and CYP2C9-so drugs that rely on those enzymes to clear from the body can build up to higher levels, leading to stronger effects or side‑effects.
Which common medications are most affected by CBD?
Warfarin (CYP2C9), clobazam (CYP2C19), many SSRIs (CYP2D6), calcium‑channel blockers, statins, and opioids like fentanyl (all CYP3A4) are among the most frequently reported.
How can I reduce the risk of sedation when using CBD with my meds?
Start CBD at a low dose, lower the dose of the interacting prescription (often 25‑50%), separate dosing times by a few hours, and monitor drug levels or clinical signs (e.g., INR for warfarin). Involving a pharmacist is also a good safety net.
Is there a safer cannabinoid alternative to CBD?
Minor cannabinoids such as CBG (cannabigerol) show far less CYP450 inhibition in lab studies, making them a potential lower‑risk option for pain or inflammation, though clinical data are still limited.
What upcoming developments might make CBD safer to use with drugs?
New nano‑formulations aim to limit CBD’s exposure to liver enzymes, and decision‑support tools like the University of Washington interaction checker are being refined to give real‑time dosing recommendations.
abidemi adekitan
October 26, 2025 AT 15:42Hey folks, great rundown! I’ve seen patients in Nigeria who started a tiny drop of broad‑spectrum CBD and had to tweak their warfarin dose by about 20 % – the key is a gentle titration and a fresh INR check after a few days.
Barbara Ventura
October 28, 2025 AT 03:53Wow!!! So many enzymes, so many meds, so much to watch!!!
Ramesh Kumar
October 29, 2025 AT 17:23Let’s dive a bit deeper into why CBD can throw a wrench into the CYP450 machinery. First, the liver enzymes act like traffic cops, directing drugs to their exit ramps; when CBD steps in, it pulls a red light on several of those cops, especially CYP3A4, CYP2C19, and CYP2C9. The inhibition isn’t just a fleeting wink – it’s a reversible block that can last as long as the CBD plasma concentration stays elevated. In practical terms, a drug that normally clears in six hours might now linger for twelve or even eighteen hours, doubling its exposure. That extended exposure is a particular nightmare for narrow‑therapeutic‑index medicines like warfarin, where a modest rise in plasma level can tip the balance from therapeutic to hazardous bleeding. The same principle applies to clobazam; its active metabolite can surge by up to 60 % when CBD is co‑administered, leading to profound sedation. Even common SSRIs such as fluoxetine can see their half‑life stretch, amplifying side‑effects like nausea or insomnia. Opioids are not exempt – fentanyl’s potency can be unexpectedly magnified, raising the risk of respiratory depression. The good news is that the effect is dose‑dependent: low‑dose CBD (under 10 mg kg⁻¹ day⁻¹) tends to produce modest enzyme inhibition, whereas higher doses push the IC₅₀ values into the clinically relevant range. Monitoring is therefore essential: check INR for warfarin, trough levels for antiepileptics, and watch for any new drowsiness or bruising. If you spot any red flags, a prudent step is to reduce the concomitant drug dose by a quarter to a half before the next lab draw. Staggering the timing – taking CBD a few hours apart from the interacting medication – can blunt the peak overlap and give the enzymes a chance to recover. Pharmacists are increasingly adding automatic alerts into dispensing software for exactly these combos. Finally, keep an eye on emerging formulations like nano‑CBD, which aim to bypass the liver and may eventually lower the interaction potential. In short, don’t panic, but do stay vigilant, communicate with your prescriber, and use labs to guide any dose tweaks.
Barna Buxbaum
October 31, 2025 AT 06:53Great points! If you’re starting CBD, a 25 % dose cut of the interacting drug is often a safe bet, and most clinicians recommend a follow‑up lab in three to five days to catch any surprises.
asha aurell
November 1, 2025 AT 20:23CBD isn’t a panacea; the enzyme blockade can be clinically significant.
Miracle Zona Ikhlas
November 3, 2025 AT 09:53Remember to keep a written list of every prescription and supplement you’re on – it makes the conversation with your pharmacist a lot smoother. Adjustments are easier when the whole team knows the full picture.
naoki doe
November 4, 2025 AT 23:23Hold on, slashing the dose without any lab data can backfire; you might end up under‑anticoagulated or lose seizure control if the reduction is too aggressive.
sarah basarya
November 6, 2025 AT 12:53Honestly, most people just ignore these warnings and then wonder why they’re suddenly out cold at dinner.
Samantha Taylor
November 8, 2025 AT 02:23Indeed, it appears that the “do‑nothing” approach is a remarkably effective strategy for achieving unintended sedation. One might suggest a proactive monitoring plan instead.
Joe Langner
November 9, 2025 AT 15:53Bottom line: stay curious, stay safe, and let the science guide your dosing – after all, a little foresight beats a lot of trouble down the road.