Combining Multiple Sedatives: The Hidden Danger of CNS Depression
 Feb, 20 2026
Feb, 20 2026
Sedative Combination Risk Calculator
Select Sedatives
Results
Physiological Effects
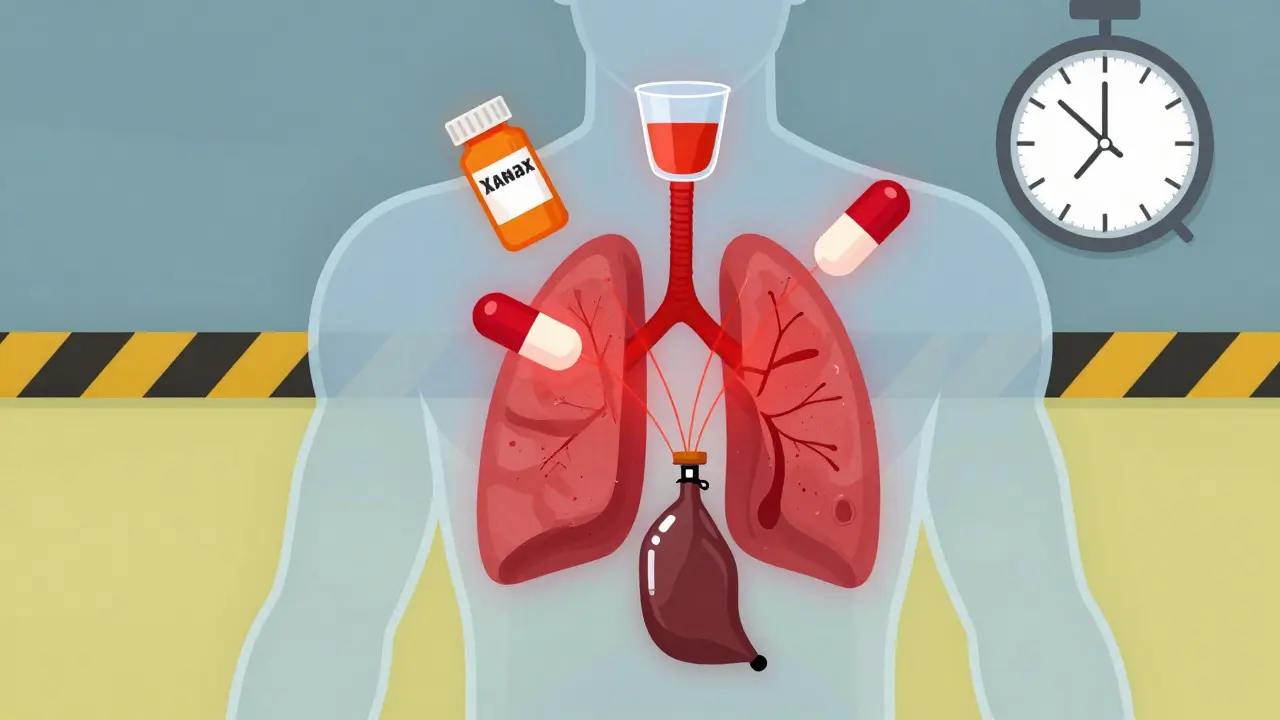
When you take one sedative, your body slows down a little. Take two? It’s not twice as slow-it’s dangerously slower. Combining multiple sedatives-whether they’re prescription, over-the-counter, or alcohol-can crash your central nervous system (CNS) into a state no one sees coming until it’s too late. This isn’t a rare accident. It’s a predictable, preventable, and deadly pattern that happens every day in homes, clinics, and hospitals around the world.
What Exactly Is CNS Depression?
Your central nervous system controls everything from breathing and heart rate to alertness and reflexes. CNS depressants don’t just make you sleepy. They silence the brain’s ability to keep your body alive. These drugs work by boosting GABA, a chemical that tells your brain to chill out. Too much GABA? Your brain stops signaling your lungs to breathe. Common CNS depressants include:- Benzodiazepines like alprazolam (Xanax), diazepam (Valium), and lorazepam (Ativan)
- Opioids like oxycodone, hydrocodone, and fentanyl
- Barbiturates (older sleep aids like phenobarbital)
- Sleep medications like zolpidem (Ambien)
- Alcohol
Each one alone can be risky. Together? They don’t just add up-they multiply.
The Deadly Math of Drug Combinations
The FDA issued a warning in 2016 after reviewing thousands of overdose cases. The message was clear: combining opioids with benzodiazepines increases the risk of death by 2.5 to 4.5 times compared to using opioids alone. That’s not a small risk. That’s a death sentence waiting to happen. Here’s what happens inside your body when you mix these drugs:- Respiratory rate drops from 12-20 breaths per minute to 4-8 breaths
- Oxygen saturation falls below 90%-sometimes under 85%
- Heart rate slows by 10-20 beats per minute
- Blood pressure drops by 15-25 mmHg
- Pupils dilate, confusion sets in, and coordination vanishes
At this point, your body can’t wake itself up. You don’t gasp. You don’t cough. You just stop breathing. Permanent brain damage can occur in 4 to 6 minutes. Death follows soon after.
Who’s Most at Risk?
This isn’t just about street drug users. It’s happening to people trying to manage pain, anxiety, or insomnia-often under a doctor’s care.- Elderly patients are 2.8 times more likely to fall and 3.4 times more likely to suffer hip fractures when taking three or more CNS depressants. The American Geriatrics Society lists 34 medications that should be avoided in seniors because of this exact risk.
- People with depression are twice as likely to mix sedatives, often using alcohol to cope with anxiety or sleep issues.
- Women are 1.7 times more likely than men to be prescribed multiple CNS depressants.
- Those with substance use disorders are 39% more likely to combine opioids with benzodiazepines or alcohol.
One study of 1,848 people on long-term opioid therapy found that nearly one-third were also taking a sedative. Among those with a history of addiction, nearly four in ten were doing it. And 12-13% of them drank alcohol within two hours of taking their opioid.
Long-Term Damage You Can’t See
The danger isn’t just overdose. Chronic use of multiple sedatives quietly destroys your body over time:- 45% of long-term users report constant fatigue
- 32% experience sexual dysfunction
- 38% develop clinical depression
- 19% have suicidal thoughts after six months of use
- 27% develop or worsen sleep apnea
- Weight gain of 12-18 pounds over a year is common
These aren’t side effects. They’re symptoms of your brain and body being chemically suppressed. Your nervous system gets lazy. It forgets how to work without drugs.
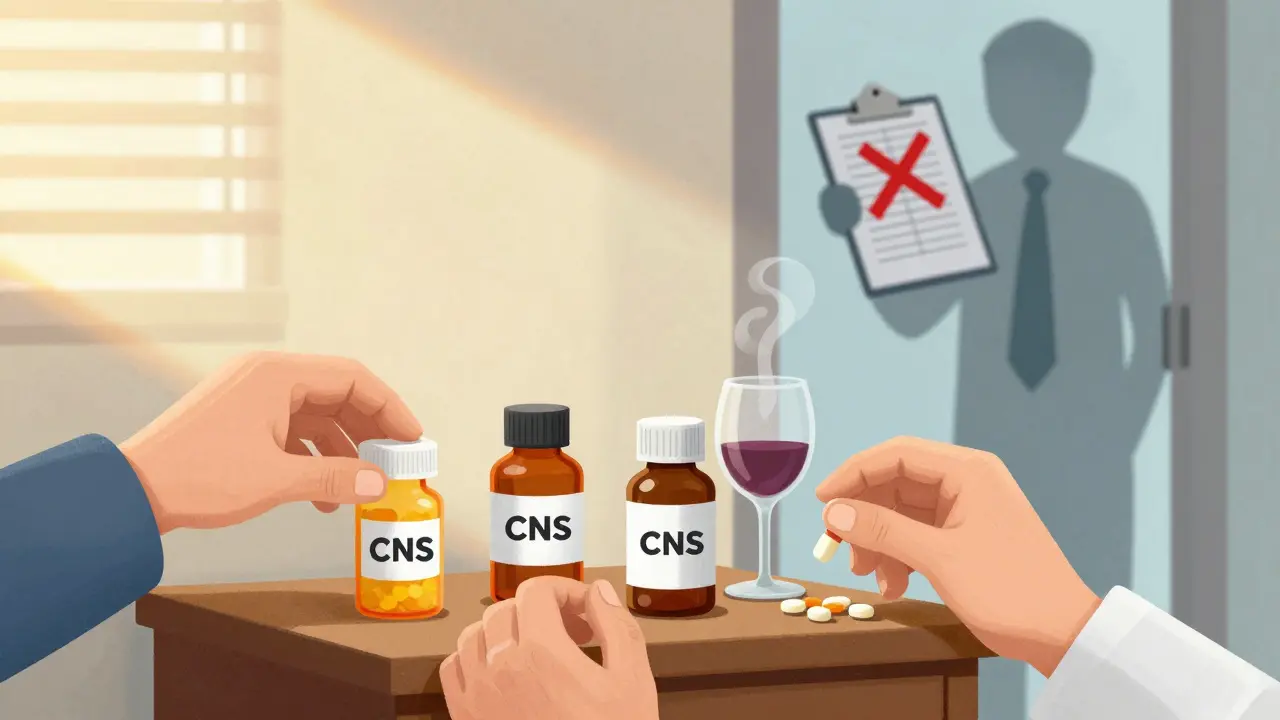
Why Do Doctors Still Prescribe These Combinations?
It’s not ignorance. It’s complexity. A 2022 study in Frontiers in Psychiatry found that 69% of hospitalizations for major depression involved more than one drug. But doctors have almost no clear guidance on which combinations are safe. Many patients get prescriptions from different specialists-a pain doctor, a psychiatrist, a sleep specialist-each unaware of the others’ prescriptions. Even worse, many patients don’t tell their doctors about alcohol use or over-the-counter sleep aids. One person might take Ambien at night, drink wine to relax, and take Xanax during the day for anxiety. They think it’s fine because each is prescribed or legal. It’s not.
What Can Be Done?
The good news? This is preventable.- Medication reviews every 3-6 months cut fall risk by 32% and reduce cognitive decline by 27% in seniors.
- Deprescribing-carefully stopping one or more drugs-has helped thousands avoid overdose. For example, switching from long-acting benzodiazepines to non-benzodiazepine sleep aids reduced ER visits by 19%.
- Electronic health records with built-in alerts can stop dangerous combinations before they happen. By 2025, most major systems will have mandatory alerts for opioid-benzodiazepine pairs.
- Pharmacogenomic testing (checking your genes for how you metabolize drugs) could reduce risky combinations by 22% in vulnerable patients.
But the most powerful tool is awareness. If you’re taking any of these drugs, ask your doctor: “Am I on more than one CNS depressant? Is this combination safe?”
What to Do If You’re Already Combining Sedatives
Don’t stop cold turkey. Withdrawal from benzodiazepines or alcohol can trigger seizures. But you don’t have to stay trapped.- Write down every medication and supplement you take-including alcohol, melatonin, and OTC sleep aids.
- Bring this list to one doctor-preferably your primary care provider-and ask them to review it.
- Ask about alternatives: Can your anxiety be treated with therapy instead of Xanax? Can your insomnia be managed with sleep hygiene instead of Ambien?
- Never drink alcohol while taking any CNS depressant. Not even one drink.
Many people feel ashamed to admit they’re mixing drugs. But this isn’t about addiction. It’s about safety. Your body doesn’t care if you’re “just” using them as prescribed. It only reacts to the chemicals.
Final Reality Check
You might think, “I’ve been doing this for years and nothing’s happened.” That’s luck, not safety. One night, one extra pill, one glass of wine, one missed appointment-and your breathing stops. No warning. No second chance. The FDA, CDC, and top medical journals all agree: combining sedatives is one of the most preventable causes of drug-related death in modern medicine. And yet, in 2020, over 10% of people on long-term opioids were still getting benzodiazepines prescribed to them-despite clear guidelines against it. This isn’t about fear. It’s about facts. And the facts are simple: more sedatives = more risk. No exceptions.Can you die from mixing alcohol and prescription sedatives?
Yes. Alcohol is a CNS depressant, and combining it with prescription sedatives like benzodiazepines, opioids, or sleep aids can cause your breathing to slow to a dangerous level-even stop. This is a leading cause of accidental overdose deaths. The risk is real even with small amounts of alcohol.
Is it safe to take two different benzodiazepines together?
No. Taking two benzodiazepines at the same time (like Xanax and Valium) multiplies the risk of overdose. They work the same way on the brain, so combining them doesn’t improve effectiveness-it just increases danger. Doctors rarely prescribe this, and when they do, it’s usually a mistake.
What should I do if I think someone is overdosing from sedatives?
Call emergency services immediately. Signs include slow or shallow breathing, unresponsiveness, blue lips or fingertips, and inability to wake up. Do not try to make them vomit or give them coffee. Keep them on their side to prevent choking. If naloxone is available and opioids are involved, administer it-but it won’t work on benzodiazepines alone. Emergency care is still critical.
Can antidepressants like SSRIs be dangerous when mixed with sedatives?
Yes. SSRIs can interfere with how your body breaks down other CNS drugs, causing them to build up to toxic levels. This is especially risky with antipsychotics, certain painkillers, and sleep aids. Studies show a high percentage of psychiatric hospitalizations involve these types of interactions, often because doctors aren’t trained to spot them.
Are there any safe combinations of sedatives?
There are no safe combinations of CNS depressants. Even if a doctor prescribes two, the risk remains. The goal is to use the fewest number of drugs possible. If you’re on more than one, ask if one can be removed or replaced with a non-drug therapy like CBT for anxiety or sleep restriction for insomnia.