Corneal Ulcers from Contact Lenses: Risks, Symptoms, and What to Do Now
 Jan, 31 2026
Jan, 31 2026
Imagine waking up with your eye burning like it’s full of sand. Your vision is blurry, light feels like a knife, and you can’t stop crying. You reach for your phone to check the time-and realize you forgot to take out your contacts last night. That’s not just discomfort. That could be a corneal ulcer.
Corneal ulcers aren’t rare. They’re one of the most dangerous complications of contact lens wear. Every year, tens of thousands of people worldwide end up in emergency eye clinics because of them. And the biggest risk factor? Sleeping in your contacts.
What Exactly Is a Corneal Ulcer?
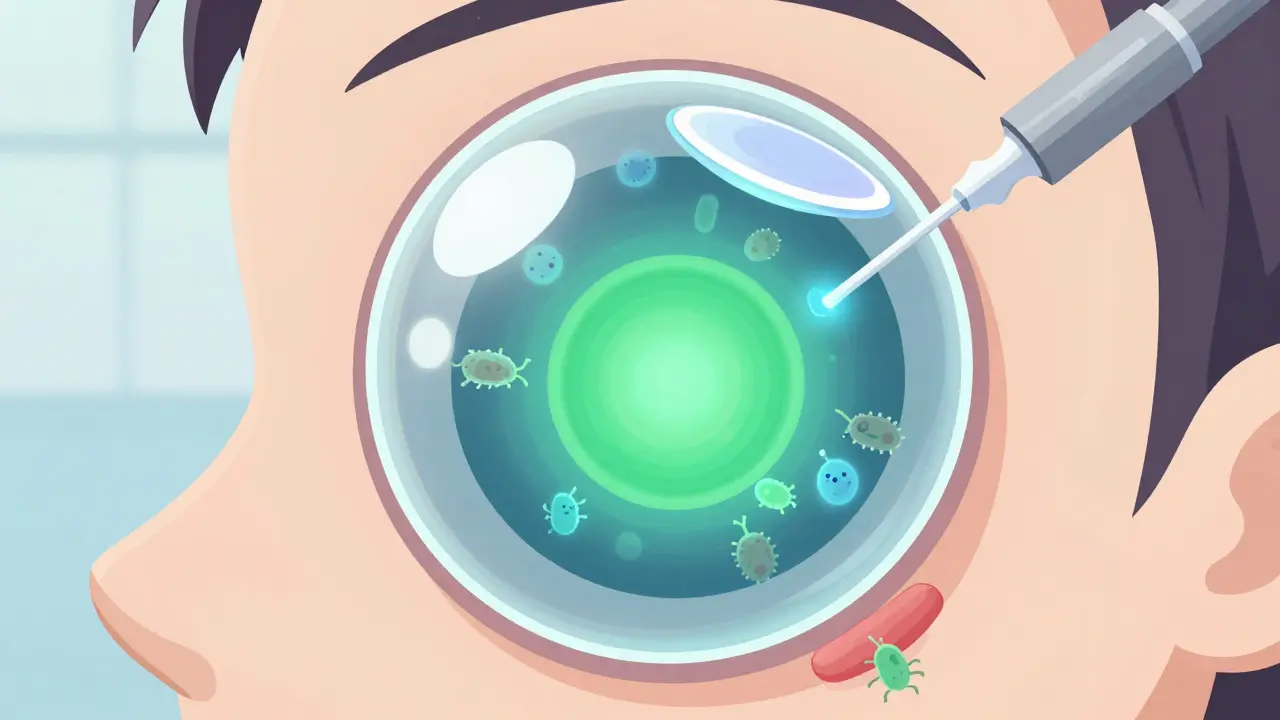
The cornea is the clear, dome-shaped surface that covers your iris and pupil. It’s not just skin-it’s a highly sensitive layer of tissue that needs oxygen, moisture, and protection. A corneal ulcer is an open sore on this surface. It’s not a scratch. It’s not a pimple. It’s tissue loss caused by infection.
Think of it like a wound on your skin that gets infected. But instead of your arm, it’s your eye. Bacteria, fungi, or even a rare amoeba called Acanthamoeba can burrow in and eat away at the cornea. Left untreated, it can scar the cornea, permanently blur your vision, or even cause blindness.
The Cleveland Clinic makes it clear: corneal ulcers are different from corneal abrasions. Abrasions are surface scratches. They hurt, sure-but they usually heal on their own in a day or two. Ulcers? They’re active infections. They demand immediate medical attention.
Why Contact Lenses Are the #1 Culprit
Over 85 million people wear contact lenses globally. Most use them safely. But even one mistake can turn a routine habit into a vision-threatening emergency.
Here’s how it happens:
- Oxygen starvation: Your cornea doesn’t have blood vessels. It gets oxygen from the air. When you wear a contact lens-especially overnight-it blocks that oxygen. The cornea starts to weaken.
- Bacteria hitchhike: Your fingers aren’t sterile. Neither are your lens cases. Even if you rinse your lenses with tap water (don’t), you’re introducing germs right onto your eye.
- Trapped debris: Dust, makeup, or a tiny scratch on your lens can create a perfect breeding ground for infection.
The numbers don’t lie. If you wear contacts, you’re about 10 times more likely to get a corneal ulcer than someone who doesn’t. But if you sleep in them? That risk jumps to 100 times higher.
Extended-wear soft lenses are the worst offenders. They’re designed to be worn overnight, but that design doesn’t make them safe. It just makes them convenient. And convenience kills eyes.
Red Flags: Don’t Wait to Act
Corneal ulcers don’t sneak up. They scream.
If you’re wearing contacts and you notice any of these, stop using your lenses right now and call your eye doctor:
- Severe eye pain-worse than any headache or sinus pressure
- Blurry or hazy vision that doesn’t clear up
- Red, bloodshot eye that looks worse than usual
- White or gray spot on the colored part of your eye (that’s the ulcer)
- Extreme sensitivity to light-even indoor lights hurt
- Excessive tearing or thick, pus-like discharge
Some people think, “I’ll just use my old antibiotic drops.” Don’t. That’s like treating a broken leg with a band-aid. The wrong treatment can make it worse.
And yes, even if you’ve had red eyes before and it went away, this isn’t the same. Ulcers progress fast. Hours matter.
How Doctors Diagnose It
Your eye doctor won’t just look and guess. They’ll use tools to confirm what’s happening.
- Fluorescein dye: A harmless orange dye is dropped in your eye. Under blue light, any damaged areas glow green. It’s like a map of the injury.
- Slit-lamp exam: A high-powered microscope lets them zoom in on the ulcer’s size, depth, and shape.
- Corneal scraping: In serious cases, they gently scrape a tiny bit of tissue from the ulcer and send it to a lab. This tells them if it’s bacterial, fungal, or amoebic.
- Visual acuity test: They check how well you can see before and after treatment.
Some clinics now use digital imaging to compare photos of your cornea over time. It helps catch early changes before the ulcer grows too big.
Treatment: Speed Is Everything
There’s no home remedy. No drops you can buy over the counter. Treatment requires prescription medication-and fast.
For most bacterial ulcers, doctors start with fluoroquinolone eye drops-powerful antibiotics like ciprofloxacin or moxifloxacin. You’ll need to use them every hour at first, then taper off as it heals.
If it’s fungal (often from contaminated water or soil), you’ll need antifungal drops like natamycin. Viral ulcers, usually from herpes simplex, are treated with antivirals like acyclovir.
Here’s the catch: if the ulcer is larger than 2 mm, or if it’s close to the center of your cornea (where you look through), it’s considered sight-threatening. In those cases, they’ll culture the sample first before choosing treatment-because the wrong drug can make it worse.
And no, you can’t use steroid drops unless your doctor specifically prescribes them. Steroids reduce swelling, but they also suppress your immune system. In an infection, that’s like giving the bacteria a free pass.
If the ulcer scars your cornea badly, you might need a corneal transplant. That’s major surgery. It’s not just expensive-it’s life-changing. And it’s 100% preventable.

How to Prevent It-For Good
The best treatment is no treatment at all. Prevention isn’t optional. It’s non-negotiable.
Here’s what actually works:
- Never sleep in your contacts. Even if they’re labeled “extended wear,” take them out. Every night. No exceptions.
- Wash your hands before touching your lenses. Soap and water. Not just wipes.
- Use only the solution your doctor recommends. Never use water, saliva, or homemade saline. Ever.
- Replace your lenses on schedule. Daily, biweekly, monthly-stick to it. Old lenses harbor bacteria.
- Replace your case every 3 months. And rinse it with solution-not water-after each use. Let it air dry upside down.
- Take your lenses out before swimming, showering, or using a hot tub. Water is the #1 source of Acanthamoeba.
- Give your eyes a break. Wear glasses at least one day a week. Let your cornea breathe.
And if you’ve ever had a corneal ulcer before? Your risk is higher next time. Be extra strict. Your vision isn’t worth gambling with.
What Happens If You Delay Care?
Some people wait a day. Or two. They think, “It’s just red. I’ll sleep on it.”
That’s how people lose vision.
Corneal ulcers can destroy the cornea in as little as 24 to 48 hours. Once the tissue is gone, it doesn’t grow back. Scar tissue forms instead. That’s permanent blurry vision. Or worse-light sensitivity that lasts for years.
The FDA warns that corneal ulcers can lead to blindness. That’s not a scare tactic. It’s a documented outcome. And it’s happening right now to people who thought they could handle it themselves.
There’s no shame in needing help. There’s only shame in waiting.
Final Reality Check
Contact lenses are amazing. They give freedom, confidence, better vision. But they’re medical devices-not accessories. They require responsibility.
You wouldn’t leave a wound on your arm untreated for days. Why treat your eye any differently?
If you wear contacts, you’re not just managing your vision. You’re managing your eye’s survival. One small habit-like taking your lenses out before bed-could be the difference between seeing clearly tomorrow… and never seeing the same way again.
Don’t wait for pain to become a warning. Listen to your eyes before they scream.
Can you get a corneal ulcer from wearing contacts for too long during the day?
Yes. Wearing contacts longer than recommended-even during the day-reduces oxygen flow and increases bacterial buildup. Daily wear lenses should be removed at night. Extended wear lenses are riskier and still require strict hygiene. Any prolonged wear increases risk.
Are daily disposable contacts safer than monthly ones?
Yes, daily disposables are the safest option for most people. Since you throw them out each day, there’s no buildup of protein, bacteria, or debris. Monthly lenses require daily cleaning and storage, which introduces more chances for contamination-even with perfect hygiene.
Can corneal ulcers heal on their own?
No. Corneal ulcers are infections that cause tissue loss. They won’t heal without treatment. Even minor ulcers can worsen rapidly. Delaying care increases the chance of permanent scarring or vision loss.
Is it safe to wear contacts while swimming?
No. Water-even from pools, lakes, or showers-contains microbes like Acanthamoeba that can cause rare but devastating infections. If you must swim with contacts, wear waterproof goggles and dispose of the lenses afterward. Never rinse lenses with tap water.
What should you do if you suspect a corneal ulcer?
Stop wearing your contacts immediately. Do not rub your eye. Do not use over-the-counter drops. Call your eye doctor right away or go to an urgent eye clinic. If it’s after hours, go to the emergency room. Time is critical-delaying treatment can cost you your vision.
Sami Sahil
February 1, 2026 AT 15:53franklin hillary
February 2, 2026 AT 04:42Naomi Walsh
February 3, 2026 AT 07:30Melissa Melville
February 3, 2026 AT 18:07Deep Rank
February 3, 2026 AT 23:29Aditya Gupta
February 4, 2026 AT 23:07Bob Cohen
February 5, 2026 AT 07:54Nancy Nino
February 6, 2026 AT 06:45Naresh L
February 8, 2026 AT 04:47