Dual Antiplatelet Therapy: How to Manage Bleeding Risks Without Compromising Heart Protection
 Dec, 26 2025
Dec, 26 2025
DAPT Bleeding Risk Calculator
Assess Your Bleeding Risk
This tool calculates your PRECISE-DAPT score based on 5 key factors. A score of 25 or higher indicates high bleeding risk (4% or greater severe bleeding chance).
Your Bleeding Risk Assessment
Score: 0
What this means
When you’ve had a heart stent placed or survived a heart attack, your doctors put you on dual antiplatelet therapy-usually aspirin plus another drug like clopidogrel, prasugrel, or ticagrelor. It’s meant to stop blood clots from forming inside the stent and causing another heart attack. But here’s the catch: the same drugs that protect your heart also make you bleed more easily. And for many people, that’s not just a minor inconvenience-it’s life-changing.
Why DAPT Works (and Why It Bleeds)
Dual antiplatelet therapy, or DAPT, blocks platelets-the tiny blood cells that stick together to form clots. Aspirin stops one pathway; the P2Y12 inhibitor blocks another. Together, they’re far more effective than either drug alone. Studies like the CURE trial showed DAPT cuts heart attacks and strokes by about 20% after a heart event.
But every time you block platelets, you’re also reducing your body’s ability to seal a cut. That’s why minor bleeding becomes a real problem. A nosebleed that lasts 15 minutes instead of 5. A bruise that spreads without a bump. A tooth extraction that keeps oozing. These aren’t rare. In fact, the TALOS-AMI trial found that 15% of patients on ticagrelor-based DAPT had what’s called ‘nuisance bleeding’-minor but frequent enough to make them stop taking their meds.
Who’s at Highest Risk for Bleeding?
Not everyone on DAPT bleeds the same way. Some people barely notice it. Others end up in the ER. Risk isn’t random. It’s predictable-and doctors now use tools to measure it.
The PRECISE-DAPT score is the most widely used tool. It looks at five things: age, history of bleeding, hemoglobin level, creatinine clearance (how well your kidneys work), and whether you’re on other blood thinners. A score of 25 or higher means you’re at high bleeding risk. That’s not a guess-it’s based on data from over 10,000 patients showing these people have a 4% or greater chance of severe bleeding in the first year.
High-risk groups include:
- People over 75
- Those with prior stomach bleeding or ulcers
- Patients with kidney disease (creatinine clearance under 60)
- Anyone with low hemoglobin (under 10 g/dL)
- People already taking warfarin, apixaban, or other anticoagulants
And here’s something many don’t realize: women, especially older women, are more likely to be classified as high bleeding risk-not because they’re weaker, but because they tend to be smaller, have lower hemoglobin, and more often have kidney issues.
The Drug Differences: Aspirin, Clopidogrel, Prasugrel, Ticagrelor
All DAPT regimens include aspirin. The variable is the second drug. And the choice matters-not just for heart protection, but for bleeding risk.
Here’s how they stack up:
| Drug Combination | Platelet Inhibition Strength | Major Bleeding Risk (vs. Aspirin Alone) | Heart Attack/Stroke Reduction | Best For |
|---|---|---|---|---|
| Aspirin + Clopidogrel | Moderate | 1.0-1.5% | 15-20% | High bleeding risk, older adults |
| Aspirin + Prasugrel | Strong | 1.8-2.2% | 20-25% | Diabetics, complex stents, lower bleeding risk |
| Aspirin + Ticagrelor | Strongest | 2.0-2.5% | 22-30% | High ischemic risk, younger patients |
Ticagrelor and prasugrel are more powerful. They work faster and more completely. But they also raise major bleeding risk by about 1% absolute compared to clopidogrel. The TRITON-TIMI 38 trial showed ticagrelor caused 27% more major bleeding than clopidogrel. That’s not a small difference-it’s enough to change treatment plans.
And here’s a real-world problem: ticagrelor causes more non-cardiac bleeding, like nosebleeds and bruising. In Reddit threads and patient surveys, people report bleeding gums, frequent nosebleeds, and cuts that won’t stop. That’s why 18.7% of patients with nuisance bleeding quit their meds within six months.
Shortening DAPT: The New Standard for High-Risk Patients
For years, the rule was simple: take DAPT for 12 months after a stent. But that’s outdated. New trials prove you don’t need to suffer bleeding for a full year if you’re at high risk.
The MASTER DAPT trial (2022) gave 3,500 high-bleeding-risk patients either 1 month of DAPT followed by aspirin alone-or the standard 12 months. At two years, the short-course group had 6.9% fewer major bleeds. No more heart attacks. No more deaths. Just less bleeding.
The Onyx ONE trial (2020) found the same thing: 1 month of DAPT, then aspirin, was safer without losing protection.
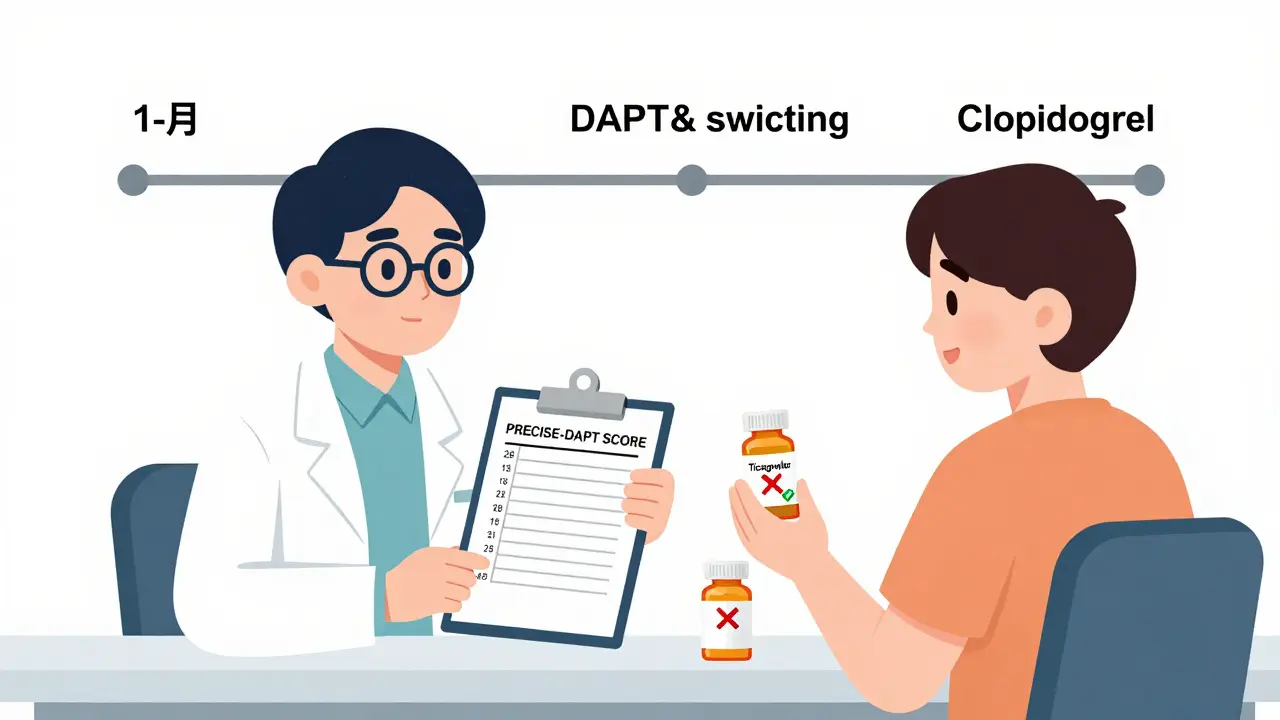
That’s why the 2023 ACC/AHA guidelines now say: if you’re high bleeding risk, start with 1 month of DAPT, then switch to aspirin alone. No need to wait 6 or 12 months.
De-Escalation: Switching to a Safer Drug
What if you’re on ticagrelor or prasugrel but you’re bleeding too much? You don’t have to quit DAPT-you can switch.
The TALOS-AMI trial tested switching from ticagrelor to clopidogrel after 1 month. Results? A 2.1% absolute drop in major bleeding events. And no rise in heart attacks. Patients felt better, too. Their quality-of-life scores jumped by 15 points on average.
This isn’t just theory. It’s now recommended in the 2022 FDA label update for ticagrelor. If you’re on a strong P2Y12 inhibitor and you’re bleeding, talk to your doctor about switching to clopidogrel after 30-90 days. It’s not giving up on protection-it’s optimizing it.

What to Do If You Start Bleeding
Not every bleed needs panic. But you need a plan.
Minor bleeding: Nosebleeds, small cuts, gum bleeding, bruising. These are common. Apply pressure. Don’t stop your meds unless your doctor says so. Most will stop on their own.
Active bleeding: Vomiting blood, black tarry stools, dizziness, fainting. Go to the ER. Don’t wait. But here’s the key: if you had a stent within the last 3 months, doctors will usually restart DAPT as soon as you’re stable. Stopping it increases stent clot risk by 2-3 times.
Procedures: You don’t need to stop DAPT for dental work, colonoscopies, or even lumbar punctures. The European Association of Percutaneous Cardiovascular Interventions says it’s safe. Only stop if you’re having major surgery with high bleeding risk-like brain or spinal surgery.
And no, platelet function tests don’t help. The French Working Group found no proof that checking platelet levels changes outcomes. Don’t waste time or money on them.
What You Can Do Right Now
If you’re on DAPT, here’s your action list:
- Ask your doctor: ‘Am I high bleeding risk?’ Get your PRECISE-DAPT score calculated.
- If you’re high risk, ask: ‘Can I switch to 1-month DAPT then aspirin alone?’
- If you’re on ticagrelor or prasugrel and bleeding, ask: ‘Can I switch to clopidogrel after 1-3 months?’
- Never stop DAPT on your own-even if you’re bleeding. Talk to your cardiologist first.
- Keep a bleeding log: note when, where, how long, and how much. Bring it to your next visit.
And if you’re feeling anxious about bleeding-don’t ignore it. That’s normal. But it’s also manageable. Patients who used de-escalation strategies reported 41% less avoidance of social activities. They slept better. They felt more in control.
The Future: Better Tools, Better Drugs
There’s no antidote yet for ticagrelor or clopidogrel. Unlike warfarin (which has vitamin K) or dabigatran (which has idarucizumab), we can’t reverse these drugs quickly. That’s why bleeding stays dangerous.
But change is coming. Two reversal agents are now in early human trials. The NIH is funding a 15,000-patient registry to predict bleeding with AI. By 2028, experts predict 90% of stent patients will get personalized DAPT plans-shorter, smarter, safer.
Right now, you don’t have to wait. The tools are here. The data is clear. You don’t have to choose between a heart attack and a bleeding emergency. You can have both protection and peace of mind.
Can I stop DAPT if I’m bleeding?
Never stop DAPT on your own. Stopping too early-especially within 6 months of a stent-doubles or triples your risk of a deadly clot forming inside the stent. If you’re bleeding, contact your doctor immediately. They’ll decide whether to pause, switch, or continue based on your risk level and timing.
Is clopidogrel less effective than ticagrelor?
Clopidogrel is slightly less potent at preventing heart attacks than ticagrelor-but the difference is small, especially after the first month. For high-bleeding-risk patients, clopidogrel offers the best balance: enough protection with far less bleeding. In fact, switching from ticagrelor to clopidogrel after 1-3 months cuts bleeding by 25-30% without increasing heart attacks.
How long should I stay on DAPT after a heart attack?
If you had a heart attack without a stent, current guidelines suggest 6-12 months of DAPT. But if you’re high bleeding risk, 6 months may be enough. If you had a stent, the rule is 6-12 months for average risk, and 1 month for high bleeding risk. Your doctor will use your PRECISE-DAPT score to decide.
Do I need to stop DAPT before dental work?
No. You do not need to stop DAPT for routine dental cleanings, fillings, or even tooth extractions. Stopping increases clot risk more than the bleeding risk from dental work. Inform your dentist you’re on blood thinners-they’ll take extra precautions, but you don’t need to pause your meds.
Why don’t we have a reversal drug for DAPT like we do for blood thinners?
Unlike anticoagulants like warfarin or dabigatran, antiplatelet drugs work by blocking platelet receptors. These receptors are complex and widespread. Creating a drug that reverses them without causing dangerous side effects has been extremely difficult. Two promising candidates are in early trials, but they’re not available yet. For now, managing bleeding means stopping the drug, waiting, or using platelet transfusions in life-threatening cases.
Managing bleeding on DAPT isn’t about avoiding risk-it’s about controlling it. With the right strategy, you can protect your heart without letting bleeding control your life.
Todd Scott
December 26, 2025 AT 14:52I’ve been on DAPT for 18 months after my stent, and let me tell you - the nosebleeds were brutal. Not the kind you pinch and it’s over. I’m talking 20-minute drips while watching TV, staining my shirts like I’d been in a horror movie. I almost quit until my cardiologist mentioned the MASTER DAPT trial. Switched to aspirin alone at 1 month, and holy hell - no more bleeding, no more panic when I brush my teeth. I’m not some medical genius, but I read the papers. The data’s clear: if you’re high-risk, 12 months isn’t sacred. It’s outdated. Your heart doesn’t need that much suppression. Your body does.
And don’t get me started on ticagrelor. It’s like giving your platelets a caffeine shot. They’re hyper, jittery, and don’t know how to chill. Clopidogrel? It’s the chill uncle who shows up with a six-pack and says, ‘We good.’ Same protection, way less drama. If your doc pushes you toward the strongest drug first, ask why. There’s a reason they make the weaker one.
Also - dental work? Don’t stop. I had three extractions on DAPT. Dentist used gauze, pressure, and a look of mild concern. I didn’t turn into a human fountain. The EAPCI guidelines are there for a reason. Use them. Stop listening to the ‘better safe than sorry’ crowd. Sometimes, safer is smarter.
And yes, I kept a bleeding log. One notebook. Red pen. Time, place, duration. Brought it to my next visit. My doc actually smiled. Said, ‘This is what patient engagement looks like.’
Stop letting fear run your meds. Let data run them.
- Todd, 63, retired ER nurse
Andrew Gurung
December 28, 2025 AT 14:13OMG. I’m so glad someone finally said it. 🙄
Of COURSE the drug companies don’t want you to shorten DAPT. They make BILLIONS off 12-month regimens. And don’t even get me started on ticagrelor - it’s basically a pharmaceutical glitter bomb for your gums. 🤢
Meanwhile, your cardiologist? Probably got a free vacation to Bali from AstraZeneca. 🏝️💸
Wake up, sheeple. This isn’t medicine. It’s a money racket. I switched to clopidogrel after 2 weeks and haven’t bled since. And guess what? Still alive. Still hearting. Still not dead. 🤷♂️
Next time your doc says ‘12 months minimum,’ ask them: ‘How much did you get paid to say that?’
Paula Alencar
December 29, 2025 AT 16:52As a nurse practitioner who has counseled over 200 patients on dual antiplatelet therapy, I feel compelled to emphasize the profound emotional burden this treatment imposes - particularly on older women, who are statistically more likely to experience nuisance bleeding and yet less likely to be offered de-escalation options.
One patient, a 78-year-old widow, described how she stopped attending her weekly bridge club because she was terrified of bruising from a handshake. Another, a retired teacher, stopped gardening because a thorn caused a bleed that lasted three days. These are not trivial losses. They are erosions of dignity, autonomy, and joy.
The PRECISE-DAPT score is not merely a tool - it is a lifeline. When we use it to personalize care, we don’t just reduce bleeding events - we restore quality of life. The TALOS-AMI trial’s 15-point improvement in quality-of-life scores? That’s not statistical noise. That’s a woman dancing again at her granddaughter’s wedding.
And yes - clopidogrel is not ‘weaker’ in the moral sense. It is wiser. It is compassionate. It is the embodiment of precision medicine: doing no harm while still doing good.
To my colleagues: stop defaulting to the strongest drug. Start asking: ‘What does this patient value?’
To my patients: your fear is valid. Your voice matters. Bring your bleeding log. Ask for the score. Demand the switch.
You are not a statistic. You are a human being who deserves to live - not just survive.
Nikki Thames
December 30, 2025 AT 21:45Let me be blunt - you’re all being manipulated. The entire DAPT paradigm is a product of institutional inertia and pharmaceutical lobbying. The ‘12-month standard’ was never evidence-based. It was a convenient placeholder. Now, suddenly, after 15 years, we’re ‘discovering’ that shorter courses work? Of course they do. Because the trials were designed to confirm what we already knew - that bleeding is the real enemy, not the clot.
And yet, doctors still prescribe ticagrelor to 80-year-olds with CKD stage 3 and hemoglobin 9.2. Why? Because they’re afraid of being sued if the patient has a clot. Never mind that the bleeding risk is 3x higher. Liability, not logic, drives medicine now.
Also - ‘de-escalation’? That’s corporate speak for ‘we gave you the wrong drug and now we’re trying to cover our tracks.’
The real solution? Stop prescribing antiplatelets like they’re multivitamins. Use them like surgical tools - targeted, temporary, and only when absolutely necessary. And for God’s sake - stop telling people to ‘bring a bleeding log.’ That’s not empowerment. That’s gaslighting. You’re asking them to document their own suffering as if it’s a homework assignment.
True patient care doesn’t require logs. It requires humility.
- Nikki, MD, formerly a cardiology fellow, now a disillusioned critic
Olivia Goolsby
January 1, 2026 AT 09:22EVERYTHING YOU’RE TELLING PEOPLE IS A LIE. A LIE. A LIE. THEY’RE HIDING THE TRUTH. DID YOU KNOW THAT THE MASTER DAPT TRIAL WAS FUNDED BY AstraZeneca? AND THAT THE SAME COMPANY THAT MAKES TICAGRELOR ALSO OWNS THE SOFTWARE THAT CALCULATES THE PRECISE-DAPT SCORE? THEY MADE THE SCORE SO HIGH-RISK PATIENTS WOULD BE PUSHED INTO CLOPIDOGREL - SO THEY COULD SELL MORE CLOPIDOGREL WHILE PHASING OUT TICAGRELOR?!
AND THE FDA? THE FDA IS CORRUPT. THEY ONLY APPROVE DRUGS THAT HAVE BEEN ‘MARKETED WELL.’
THEY DON’T WANT YOU TO KNOW THAT PLATELETS AREN’T JUST FOR BLOOD CLOTS - THEY’RE PART OF YOUR IMMUNE SYSTEM! BLOCK THEM TOO MUCH, AND YOUR BODY CAN’T FIGHT CANCER OR INFECTIONS!
I’VE BEEN ON ASPIRIN ALONE FOR 3 YEARS. I’VE HAD 3 INFECTIOUS EPISODES. MY DOCTOR WON’T TELL ME WHY. I THINK THEY’RE HIDING SOMETHING.
AND THE ‘NO REVERSAL DRUG’ THING? THEY HAVE ONE. THEY JUST WON’T RELEASE IT. BECAUSE IF YOU COULD REVERSE IT, YOU COULD SELL IT FOR $10,000 A DOSE. THEY’RE PROFITING OFF YOUR FEAR.
THEY’RE LYING TO YOU. THEY’RE LYING TO YOUR DOCTOR. THEY’RE LYING TO EVERYONE.
WHY DO YOU THINK THEY CALL IT ‘DUAL ANTIPLATELET THERAPY’? BECAUSE THEY WANT YOU TO THINK IT’S TWO DRUGS - BUT IT’S ONE SYSTEM. ONE CONTROLLED SYSTEM. ONE SYSTEM THAT WANTS YOU TO BELIEVE YOU NEED IT FOREVER.
WAKE UP.
THEY’RE NOT HELPING YOU.
THEY’RE CONTROLLING YOU.
Nicola George
January 2, 2026 AT 08:46Y’all are acting like this is some new revelation. Been on clopidogrel since 2019 after my MI. Blew out a knee cap last year - no bleeding. Got a root canal? No drama. My doctor said ‘1 month then aspirin’ and I was like ‘cool, thanks.’
Meanwhile, my cousin? On ticagrelor. Had to cancel her niece’s wedding because she was ‘too bruised to wear a dress.’
So yeah - it’s not rocket science. It’s just common sense. And apparently, that’s the rarest drug in cardiology.
Raushan Richardson
January 2, 2026 AT 23:05I’m so glad this thread exists. I was terrified to even ask my doctor about switching - felt like I was being ‘difficult.’ But after reading this, I went in with my bleeding log (yes, I kept one - 3 nosebleeds in 2 weeks, 2 gum bleeds after brushing, one huge bruise from hugging my dog) and asked if I could switch to clopidogrel after 1 month. She said ‘YES’ and even high-fived me. 😭
It’s not about being weak. It’s about being smart. And I’m so proud of myself for speaking up. If you’re scared - you’re not alone. But you’re also not powerless. Ask. Bring the data. You’ve got this.
Robyn Hays
January 3, 2026 AT 18:37I love how this thread turned from clinical jargon into a collective sigh of relief. Like, we’ve been living in this fog of ‘more is better’ for so long - and then someone says, ‘Actually, less can be more,’ and suddenly the clouds part.
It’s not just about bleeding. It’s about reclaiming the mundane. The quiet joy of shaving without checking your face for blood. The peace of sleeping without wondering if you’ll wake up to a nosebleed. The dignity of holding your grandchild without fear of bruising their skin.
And clopidogrel? It’s not a downgrade. It’s a recalibration. Like switching from a sledgehammer to a scalpel. Same goal - just less collateral damage.
Also - the ‘no reversal drug’ thing? It’s not a flaw. It’s a feature of biology. Platelets aren’t pills you can undo. They’re living cells. We’re trying to tame a biological storm with a teaspoon. Maybe we should stop trying to control everything - and start working with the body, not against it.
Thank you for this. I needed to read it.
Liz Tanner
January 5, 2026 AT 01:05Just wanted to say thank you to the person who mentioned the bleeding log. I started one last week after my 2nd nosebleed in 48 hours. I didn’t think it mattered. But I wrote down: ‘July 12 - 8:15 AM, right nostril, 12 min, pressure applied, stopped.’
I brought it to my appointment. My doctor said, ‘This is the first time a patient has done this.’ Then she pulled up my PRECISE-DAPT score - 31. High risk.
She switched me to clopidogrel. We’re doing 1-month DAPT.
I cried in the parking lot.
You’re not alone. And your voice matters.
Babe Addict
January 6, 2026 AT 09:11Let’s cut through the noise. DAPT isn’t about ‘personalization.’ It’s about pharmacokinetics. Ticagrelor has a 7-12 hour half-life. Clopidogrel is 15-20 hours. Prasugrel? 3-7 hours. The bleeding risk correlates with CYP2C19 metabolism, not ‘risk scores.’ The PRECISE-DAPT score is just a proxy for age and renal function - which are proxies for polypharmacy and frailty.
And the ‘switching’ data? It’s confounded by adherence. Patients on ticagrelor have higher discontinuation rates because of dyspnea - not bleeding. So when they switch to clopidogrel, they feel better - but it’s not the drug, it’s the placebo effect of stopping the one that made them feel like they’re suffocating.
Also - platelet function testing? It’s useless. But not because it doesn’t work. Because it’s not standardized. The VerifyNow assay has a 25% CV. You can’t base clinical decisions on that.
So yes - shorten DAPT. Switch drugs. But don’t pretend it’s magic. It’s pharmacology. And we still don’t understand half of it.
Satyakki Bhattacharjee
January 7, 2026 AT 03:17People are too focused on bleeding. But what about the soul? When you take medicine, you are not just treating the body. You are fighting the spirit. The heart is not just a pump. It is the seat of life. To block its protection is to block God's will.
I am from India. In my village, we use neem leaves and turmeric. They heal the blood. Why do we need Western drugs? They are too strong. They hurt the body too much.
Maybe the real answer is not to change the drug - but to change the heart.
Pray. Eat clean. Live simple.
Then the blood will flow as it should.