Fluticasone Nasal Spray for Non-Allergic Rhinitis: Benefits, Dosage & Side Effects
 Oct, 18 2025
Oct, 18 2025
Fluticasone Nasal Spray Dosage Calculator
This tool helps determine the correct fluticasone nasal spray dosage based on age and symptoms.
This is the standard dose for your condition. Always consult your doctor before starting treatment.
Expected relief: In most patients, relief begins within 2-3 days and peaks at about 2 weeks of consistent use.
Ever wonder why your nose stays congested even when pollen counts are low? That stubborn stuffiness often points to non‑allergic rhinitis, a condition that sneaks up on you without the classic allergy triggers. Fluticasone nasal spray has become a go‑to remedy, but many patients aren’t sure how it works, how to use it correctly, or whether it’s the right choice for them.
What Is Non-Allergic Rhinitis?
Non-allergic rhinitis is a chronic inflammation of the nasal passages that occurs without an IgE‑mediated allergic response. Common triggers include changes in temperature, strong odors, spicy foods, and hormonal fluctuations. Unlike allergic rhinitis, skin‑prick tests and specific IgE panels are usually negative.
Symptoms typically involve persistent nasal congestion, rhinorrhea (runny nose), and post‑nasal drip. Because the condition isn’t driven by histamine release, antihistamines often provide limited relief, prompting doctors to look at alternative therapies.
How Fluticasone Nasal Spray Works
Fluticasone nasal spray is a prescription‑strength intranasal corticosteroid that reduces inflammation by binding to glucocorticoid receptors in the nasal mucosa. Once attached, the drug suppresses the production of inflammatory cytokines, shrinking swollen tissue and decreasing mucus production.
The molecule’s high topical potency and low systemic bioavailability mean you get strong local effects with minimal risk of affecting the hypothalamic‑pituitary‑adrenal (HPA) axis. In clinical trials, twice‑daily dosing lowered nasal symptom scores by up to 60% after two weeks.
Recommended Dosage & Administration Tips
For adults and children 12 years or older, the typical regimen is two sprays in each nostril once daily (about 50 µg per spray). Some physicians start with one spray per nostril for the first few days to gauge tolerance.
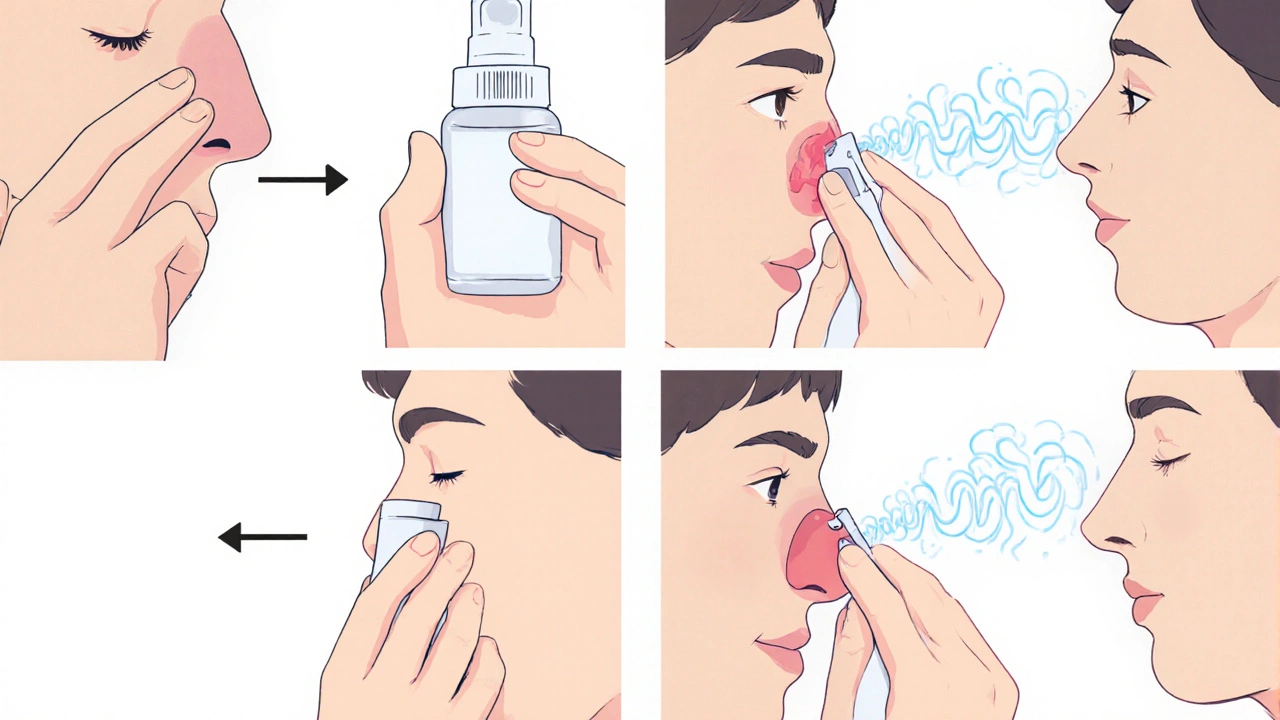
- Blow your nose gently to clear excess mucus.
- Shake the bottle for 5 seconds.
- Close one nostril with a finger, insert the tip, and aim the spray toward the outer wall of the opposite nostril (not straight up). This maximizes coverage of the turbinate region.
- Repeat on the other side, then avoid blowing the nose for at least 15 minutes.
- Use the same time each day to build a routine.
Consistent use is key; missing doses can lead to a rebound of symptoms. If you’re switching from another intranasal steroid, a brief overlap (2-3 days) is safe, but check with your clinician.
Benefits Compared to Other Treatment Options
Because non‑allergic rhinitis isn’t driven by histamine, oral antihistamines often fall short. Oral antihistamines are medications that block H1 receptors, primarily useful in allergic rhinitis. In contrast, intranasal corticosteroids directly target the inflamed tissue.
Below is a quick comparison of the most common intranasal steroids used for rhinitis.
| Drug | Typical Daily Dose | Onset of Relief | Key Side Effects |
|---|---|---|---|
| Fluticasone | 100 µg (2 sprays/nostril) | 2-3 days | Nasal irritation, rare epistaxis |
| Mometasone | 200 µg (2 sprays/nostril) | 3-5 days | Headache, throat dryness |
| Budesonide | 128 µg (2 sprays/nostril) | 4-7 days | Fungal growth, taste alteration |
Fluticasone’s lower dose and faster onset make it a popular first‑line choice for many patients.
Common Side Effects & Safety Considerations
While intranasal corticosteroids are generally safe for long‑term use when administered at recommended dosages, a few cautions are worth noting:
- Nasal irritation or burning: Often mild and improves after a week.
- Epistaxis (nosebleeds): Use a saline rinse if bleeding occurs.
- Potential impact on the HPA axis: Rare at low doses, but clinicians may monitor cortisol levels in patients using high‑dose or prolonged therapy.
- Ocular effects: Very low risk of elevated intra‑ocular pressure, but patients with glaucoma should discuss with their ophthalmologist.
Systemic absorption is less than 1% of the oral dose, so you’re unlikely to experience classic steroid side effects like weight gain or mood swings.
Practical Tips for Long‑Term Use
Success with fluticasone isn’t just about the medication; it’s also about the routine around it.
- Combine with saline irrigation: A daily rinse clears mucus, allowing the spray to coat the mucosa more evenly. Nas al saline irrigation is a non‑medicinal method that helps keep nasal passages moist and reduces crusting.
- Avoid over‑use: More than the prescribed number of sprays won’t speed relief and may increase irritation.
- Monitor symptoms: Keep a brief diary for the first two weeks-note congestion scores, any bleeding, or throat dryness.
- Check technique annually: Improper spray angle can deposit medication on the septum, causing irritation.
If symptoms persist after 4-6 weeks despite correct use, discuss alternate therapies such as a short course of oral steroids or referral to an ENT specialist for possible structural issues.
Frequently Asked Questions
Can I use fluticasone if I’m pregnant?
Current guidelines categorize fluticasone as a Category B drug for pregnancy, meaning animal studies show no risk but human data are limited. Discuss risks with your obstetrician; many doctors still prescribe it when the benefits outweigh the potential risks.
How long does it take to feel relief?
Most patients notice a reduction in congestion within 2-3 days, with maximal benefit around the 2‑week mark.
Is there a risk of “rebound congestion” after stopping?
Rebound congestion is more common with decongestant sprays like oxymetazoline. With fluticasone, tapering over a week or two is usually enough to prevent any sudden return of symptoms.
Can children use fluticasone nasal spray?
The FDA approves fluticasone for children 4 years and older for allergic rhinitis. For non‑allergic rhinitis, doctors often use the same dosing but will confirm safety on a case‑by‑case basis.
What should I do if I develop a nosebleed?
Stop the spray, sit upright, and apply gentle pressure to the soft part of the nose for 5‑10 minutes. Using a saline rinse and a humidifier can help prevent future bleeds.
Whether you’re newly diagnosed with non‑allergic rhinitis or have been struggling with chronic congestion for years, understanding how fluticasone nasal spray works, how to use it correctly, and what to expect can make the difference between a stubborn blocked nose and a clear, comfortable airway.
Fabian Märkl
October 18, 2025 AT 18:48Wow, Fluticasone nasal spray really seems like a game‑changer for non‑allergic rhinitis! 🚀 If you get the technique right, you’ll notice the congestion melt away in just a few days. Remember to shake the bottle and aim the spray toward the outer wall of the nostril – that’s the sweet spot for maximum coverage 😊.
Avril Harrison
November 3, 2025 AT 13:00Nice rundown, especially the tip about waiting 15 minutes before blowing your nose. Keeps the medication where it belongs.
Natala Storczyk
November 19, 2025 AT 08:12This is the ultimate guide!!! Fluticasone isn’t just another spray, it’s the *weapon* against chronic stuffiness!!! Follow the dosing schedule and you’ll crush those relentless nasal blockages!!!
Sarah Hanson
December 5, 2025 AT 03:24Thank you for the thorough overview; the instructions are clear and helpful, despite a few minor typos such as teh dosage.
Karla Johnson
December 20, 2025 AT 22:36Fluticasone nasal spray works by binding to glucocorticoid receptors in the nasal mucosa and suppressing inflammatory cytokines.
This mechanism addresses the underlying inflammation that characterizes non‑allergic rhinitis rather than merely masking symptoms.
Clinical studies have shown that patients experience a reduction in congestion scores by up to 60 percent within two weeks of consistent use.
The recommended adult dosage of two sprays per nostril once daily delivers approximately 100 µg of medication, which is sufficient for most individuals.
Starting with a single spray per nostril for the first few days can help assess tolerance and minimize local irritation.
Proper administration technique, such as shaking the bottle, gently clearing the nostrils, and aiming the spray toward the outer nasal wall, maximizes mucosal coverage.
It is also advisable to avoid blowing the nose for at least fifteen minutes after each application to allow the drug to adhere.
Combining the spray with a daily saline irrigation can further enhance distribution and reduce crusting.
Patients should monitor for mild side effects like nasal dryness or occasional epistaxis, and use a humidifier or saline rinse if these occur.
Rarely, systemic absorption may occur, but it remains below one percent of oral steroid exposure, keeping systemic effects minimal.
For individuals with glaucoma or a history of ocular hypertension, a consultation with an ophthalmologist is prudent before starting therapy.
In cases where symptoms persist beyond six weeks despite correct usage, physicians may consider a brief course of oral steroids or refer the patient to an ENT specialist.
The cost of fluticasone has become more manageable with the availability of generic formulations, making long‑term adherence more feasible.
Insurance coverage varies, so checking formularies and prior‑authorization requirements can prevent unexpected out‑of‑pocket expenses.
Education on proper technique is essential; many patients inadvertently spray onto the septum, which can cause irritation and bleeding.
Ultimately, when used correctly, fluticasone offers a safe, effective, and convenient option for controlling the burdensome symptoms of non‑allergic rhinitis.
Grace Hada
January 5, 2026 AT 17:48In the grand schema of nasal health, fluticasone stands as a rational choice; use it wisely.
alex montana
January 21, 2026 AT 13:00Fluticasone is powerful!!! you just gotta use it right??? no doubt its effect is real
Wyatt Schwindt
February 6, 2026 AT 08:12Proper technique makes all the difference
Lyle Mills
February 22, 2026 AT 03:24Intranasal corticosteroid delivery optimizes mucosal anti‑inflammatory pathways while minimizing systemic glucocorticoid load