Glaucoma: Understanding Elevated Eye Pressure and Optic Nerve Damage
 Jan, 23 2026
Jan, 23 2026
Glaucoma doesn’t come with warning signs. No pain. No redness. No blurry vision-until it’s too late. By the time most people notice something’s wrong, they’ve already lost up to 40% of their peripheral vision. That’s the quiet danger of glaucoma: it steals sight silently, one nerve fiber at a time. And it’s not just about high eye pressure. While elevated intraocular pressure (IOP) is the most common trigger, it’s not the whole story. Many people with normal pressure still lose vision. Others with pressure above 30 mmHg never develop damage. So what’s really going on?
What Happens When Eye Pressure Rises
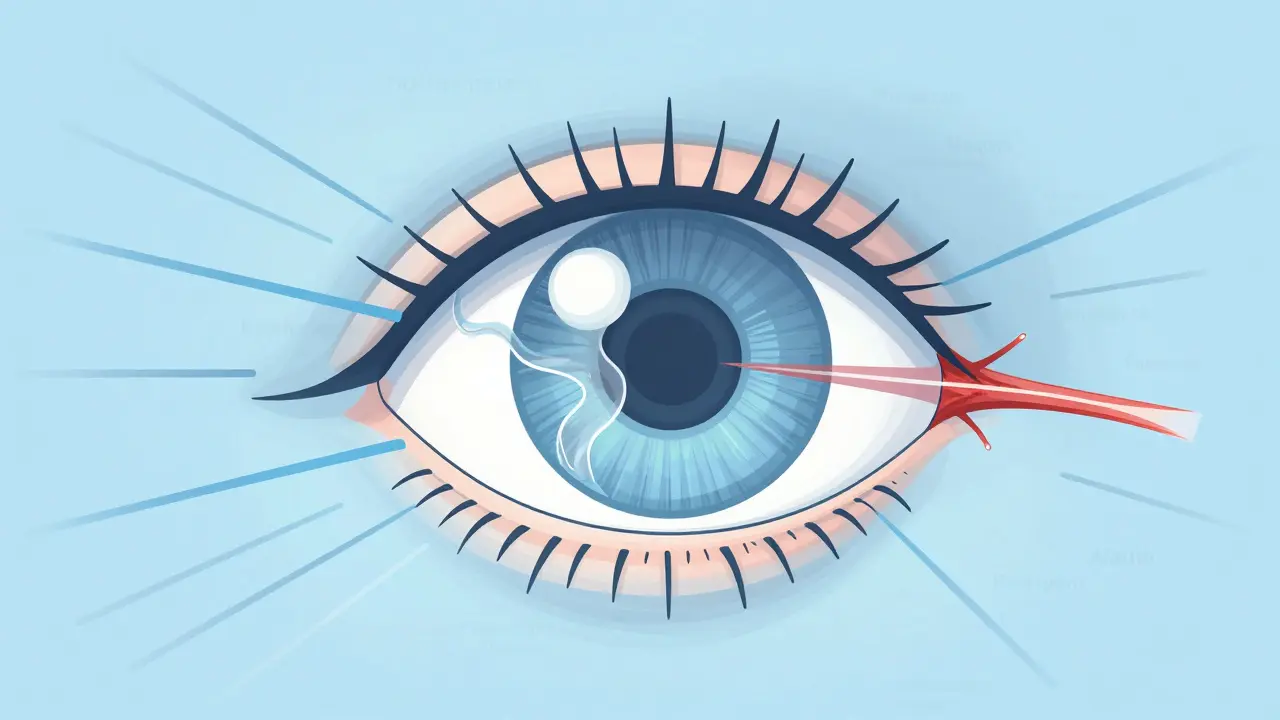
Your eye is a fluid-filled sphere. Inside, a clear liquid called aqueous humor flows in and out, keeping pressure steady. Normal pressure? Between 10 and 21 mmHg. Anything above that, especially if it stays high for years, starts putting stress on the back of your eye-specifically, the optic nerve head. This is where the real damage begins. The optic nerve is made up of over a million tiny nerve fibers that carry visual information from your retina to your brain. These fibers pass through a sponge-like structure called the lamina cribrosa. When pressure builds up, this structure gets stretched. Think of it like pulling a net too tight-it starts to deform. Studies using advanced imaging show that in glaucoma patients, the lamina cribrosa moves backward up to 50% more than in healthy eyes. That mechanical strain crushes the nerve fibers, cutting off their ability to send signals. The cells that die first are the retinal ganglion cells. Once they’re gone, they don’t come back. That’s why vision loss from glaucoma is permanent. And here’s the kicker: this damage doesn’t happen overnight. It creeps in over years, often without you noticing. By the time you miss a step on the stairs or bump into doorframes, the damage is already advanced.It’s Not Just About Pressure
Not everyone with high eye pressure gets glaucoma. And not everyone with glaucoma has high pressure. That’s where normal-tension glaucoma (NTG) comes in. In NTG, eye pressure stays below 21 mmHg-sometimes even under 15 mmHg-but the optic nerve still gets damaged. Why? Research points to a pressure imbalance between your eye and your brain. The fluid surrounding your brain, called cerebrospinal fluid, has its own pressure. In healthy people, the pressure inside the eye and the pressure behind the eye are roughly balanced. But in glaucoma patients, especially those with NTG, brain pressure is often lower than normal-around 9.7 mmHg compared to 13.7 mmHg in people without glaucoma. That means the difference between eye pressure and brain pressure (called the translaminar pressure gradient) becomes too large. Even if your eye pressure is "normal," if your brain pressure is low, your optic nerve still gets squeezed from the inside out. This explains why some people with pressure at 25 mmHg never develop glaucoma-they might have higher brain pressure. And why others with pressure at 14 mmHg still lose vision-they might have low brain pressure. It’s not just the number on the tonometer. It’s the balance.Types of Glaucoma You Need to Know
There are three main types, each with different causes and risks:- Primary Open-Angle Glaucoma (POAG)-This is the most common form, making up about 90% of cases in the U.S. The drainage angle of your eye looks normal, but the fluid drains too slowly. Pressure builds up gradually. It’s slow, silent, and sneaky.
- Normal-Tension Glaucoma (NTG)-About 20-30% of cases in Western countries, but up to 70% in parts of Asia. Damage happens even when pressure is in the normal range. Often linked to low cerebrospinal fluid pressure, poor blood flow to the optic nerve, or autoimmune factors.
- Angle-Closure Glaucoma-This one is urgent. The drainage angle suddenly gets blocked, causing pressure to spike fast. Symptoms include severe eye pain, nausea, blurred vision, and halos around lights. It’s rare globally but causes half of all glaucoma-related blindness in Asia because it often goes undetected until it’s an emergency.

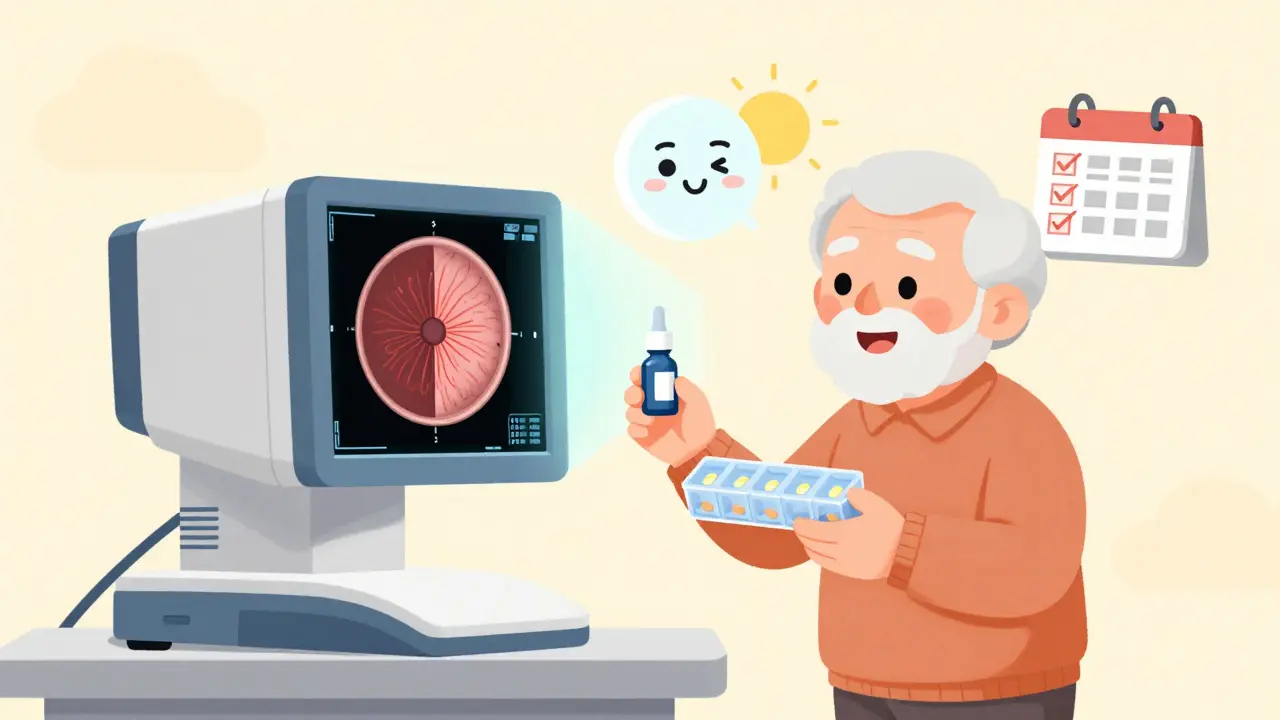
How Doctors Catch It Early
The only way to stop glaucoma before it steals your vision is to catch it early. And that means regular eye exams-especially after age 40. Here’s what your eye doctor checks:- Intraocular pressure-Measured with a Goldmann tonometer, the gold standard. It’s quick, painless, and gives the most accurate reading.
- Optic nerve imaging-Using optical coherence tomography (OCT), doctors can see thinning in the retinal nerve fiber layer as small as 5-10 microns. That’s thinner than a human hair.
- Visual field testing-The Humphrey perimeter test maps your peripheral vision. It detects tiny blind spots as small as 1 dB of sensitivity loss. You’ll stare at a light while flashes appear around you. It’s boring, but it’s your best defense.
- Eye drainage angle exam-A gonioscopy lens lets the doctor see if the drainage channel is open, narrow, or blocked.
What Treatments Actually Work
The goal isn’t to cure glaucoma. It’s to stop it from getting worse. And the only proven way to do that is to lower eye pressure.- Eye drops-First-line treatment. Prostaglandin analogs like latanoprost reduce pressure by 25-33% with just one drop a day. But they can cause darkening of the iris, longer eyelashes, and sunken eyes over time. About 1 in 5 people stop using them because of side effects.
- Laser treatment-Selective laser trabeculoplasty (SLT) opens up the drainage system. It works in 75% of people, lowering pressure by 20-30%. But its effect fades over time-about 10% per year. It’s safe, quick, and can be repeated.
- Surgery-If drops and laser fail, surgery is next. Trabeculectomy creates a new drainage channel. It works well for years, but 1 in 5 people develop complications like infection or low pressure. Newer micro-invasive glaucoma surgeries (MIGS), like iStent, are safer but offer smaller pressure drops-around 20-25%.
What’s on the Horizon
Scientists are looking beyond pressure. New research shows that some drugs might protect nerve cells directly-without lowering IOP at all. The LIBERTI study found that brimonidine, a common glaucoma drop, slowed vision loss in NTG patients by 30% compared to timolol-even when both drops lowered pressure equally. That suggests it’s doing more than just reducing pressure. It might be protecting the optic nerve. Other promising ideas:- Neuroprotection-Experiments with oncomodulin and CNTF (a growth factor) have regrown damaged nerve fibers in animals. Human trials are starting.
- Gene therapy-Early trials inject genes into the eye to improve fluid drainage. One study showed a 25% pressure drop lasting six months.
- Home monitoring-New contact lenses like the Triggerfish sensor measure eye pressure continuously for 24 hours. That’s huge-because pressure spikes often happen at night or early morning, when you’re not at the doctor’s office.
- AI analysis-Machine learning can now detect early glaucoma from OCT scans with 94% accuracy. It spots changes humans miss.
Living With Glaucoma
Glaucoma isn’t a death sentence. But it’s a lifelong condition. You’ll need checkups every 3 to 6 months. You’ll need to take drops daily-even if you feel fine. And you’ll need to stay calm. A 2022 survey of 1,200 glaucoma patients found that 68% lived with constant fear of going blind. That’s understandable. But the truth is, with proper treatment, most people keep their vision for life. One patient in a Glaucoma.org forum shared that after a trabeculectomy, his pressure dropped from 32 to 14 mmHg-and his vision hasn’t changed in 10 years. The hardest part? Adherence. Half of patients stop taking their drops within a year. Side effects, forgetfulness, or thinking "I feel fine" are the reasons. But here’s the hard truth: if you skip your drops, your vision will keep fading. No exceptions.What You Can Do Today
If you’re over 40, get a comprehensive eye exam-even if you have perfect vision. If you have a family history, start at 35. Don’t wait for symptoms. Glaucoma doesn’t give you a heads-up. If you’ve been diagnosed:- Take your drops exactly as prescribed-even if your pressure seems normal.
- Ask your doctor for OCT scans and visual field tests every year.
- Keep your blood pressure and blood sugar under control.
- Don’t smoke. Smoking reduces blood flow to the optic nerve.
- Exercise regularly. Moderate aerobic activity lowers IOP by 5-10 mmHg for hours after.
- Don’t panic about your numbers. Focus on consistency. Stability beats perfection.
Luke Davidson
January 24, 2026 AT 22:52Alexandra Enns
January 25, 2026 AT 17:15Marie-Pier D.
January 26, 2026 AT 06:37Marlon Mentolaroc
January 26, 2026 AT 15:37Josh McEvoy
January 27, 2026 AT 11:25Gina Beard
January 29, 2026 AT 01:01Helen Leite
January 30, 2026 AT 14:04Phil Maxwell
January 30, 2026 AT 19:46Tiffany Wagner
January 31, 2026 AT 08:40siva lingam
January 31, 2026 AT 13:41Darren Links
February 1, 2026 AT 18:39Kat Peterson
February 3, 2026 AT 18:05Don Foster
February 5, 2026 AT 04:09Shelby Marcel
February 5, 2026 AT 06:36Tommy Sandri
February 5, 2026 AT 17:19