Grapefruit Juice Interactions: Why Some Medications Are Affected
 Dec, 19 2025
Dec, 19 2025
One glass of grapefruit juice in the morning might seem like a healthy choice-until it starts interfering with your medication. For people taking certain prescriptions, that refreshing citrus drink could be hiding a dangerous secret. It doesn’t matter if it’s fresh-squeezed, from a carton, or eaten straight from the fruit. The effect is the same: grapefruit juice can turn a safe dose of medicine into a risky, even life-threatening one.
How Grapefruit Juice Changes How Your Body Handles Medication
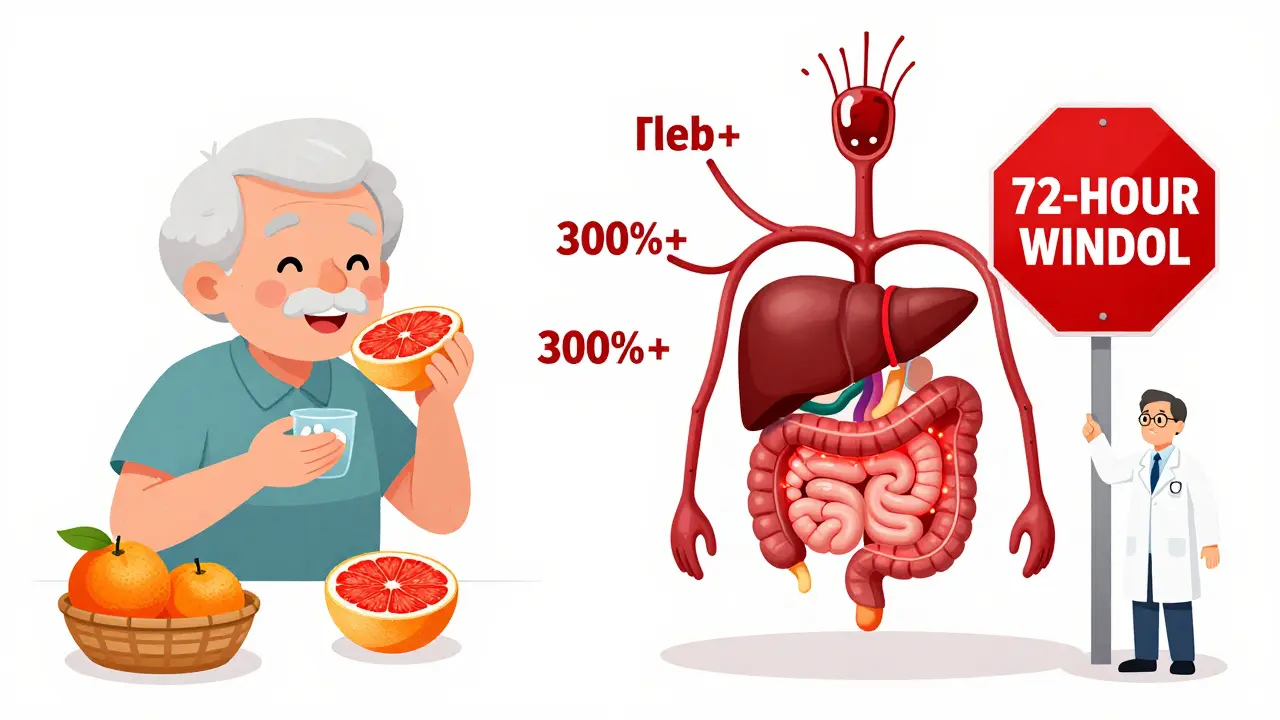
The problem isn’t about the sugar or acidity. It’s about chemicals called furanocoumarins, mainly bergamottin and 6',7'-dihydroxybergamottin, found naturally in grapefruit. These compounds attack an enzyme in your gut called CYP3A4. This enzyme normally breaks down many medications before they enter your bloodstream, keeping their levels in check.
When grapefruit juice shuts down CYP3A4, your body can’t break down the drug properly. Instead of 50% being filtered out, now 80%, 90%, or even more gets absorbed. That means your blood ends up with much higher drug levels than intended. For some medications, that’s like taking three or four pills at once-without knowing it.
This isn’t a temporary glitch. The enzyme doesn’t just slow down-it gets permanently damaged. Your body needs about 72 hours to grow new enzymes and restore normal function. So even if you drink grapefruit juice at breakfast and take your pill at night, the damage is already done.
Which Medications Are Most at Risk?
Not all drugs are affected. But for those that are, the consequences can be serious. The FDA lists over 85 medications with known grapefruit interactions, and about 43 of them carry a high risk of harm.
Statins, used to lower cholesterol, are one of the most common culprits. Simvastatin and lovastatin can cause dangerous muscle damage (rhabdomyolysis) when their levels spike. A single 200mL glass of grapefruit juice can boost simvastatin levels by 330%. Atorvastatin is also affected, but pravastatin, rosuvastatin, and fluvastatin are safe-because they’re processed differently.
Calcium channel blockers like felodipine and nifedipine can cause your blood pressure to drop too low, leading to dizziness, fainting, or even heart problems. Felodipine levels can jump 300% to 800% after grapefruit juice. Amlodipine, however, isn’t affected at all.
Other high-risk drugs include:
- Immunosuppressants like cyclosporine and tacrolimus (risk of kidney damage)
- Antiarrhythmics like amiodarone (risk of irregular heartbeat)
- Benzodiazepines like midazolam (risk of excessive sedation)
- Some antidepressants and antipsychotics, including sertraline and quetiapine
- ED medications like sildenafil (Viagra) - can cause dangerously low blood pressure
Some drugs behave oddly-like theophylline or itraconazole-where grapefruit juice actually lowers their levels, making them less effective. The reason isn’t fully understood, but it’s another reminder: don’t assume grapefruit is harmless just because your drug isn’t on the "danger list."
Why Some People Are More at Risk Than Others
Not everyone reacts the same way. One person might drink grapefruit juice with their statin and feel fine. Another might end up in the hospital. Why?
It comes down to biology. People naturally have different levels of CYP3A4 in their intestines. Those with higher baseline levels see the biggest spikes in drug concentration-sometimes up to eight times higher. Genetics also play a role. A variant called CYP3A4*22 makes some people far more sensitive to grapefruit’s effects.
Age matters too. Older adults are at higher risk because they’re more likely to be on multiple medications and have slower metabolism. About 42% of adults over 65 take five or more drugs-and many of them are on grapefruit-sensitive ones. The American Geriatrics Society includes grapefruit interactions in their 2023 Beers Criteria as a key concern for seniors.
And here’s the scary part: most people don’t know they’re at risk. A 2021 study found only 28% of patients could correctly name which of their meds were affected-even after being told by a pharmacist.
What About Other Citrus Fruits?
Not all citrus is dangerous. Regular oranges, tangerines, and clementines are safe. They don’t contain enough furanocoumarins to cause problems.
But Seville oranges-used in marmalade-and pomelos are just as risky as grapefruit. They have similar levels of the same chemicals. So if you’re on a high-risk medication, skip the orange marmalade on your toast.
Limes and lemons? Generally safe. There’s no strong evidence they affect CYP3A4 at normal consumption levels. But if you’re unsure, stick to what’s confirmed: orange, tangerine, and mandarin are your safest bets.
What Should You Do?
If you’re taking any prescription medication, here’s what to do:
- Check your label. Look for warnings about grapefruit juice. About 20% of U.S. prescription labels now include this warning, up from 12% in 2015.
- Ask your pharmacist. They’re trained to spot these interactions. Don’t assume they’ll bring it up-ask directly: "Does my medication interact with grapefruit?"
- Don’t just avoid juice-avoid the fruit too. One whole grapefruit contains enough furanocoumarins to cause the same effect as a glass of juice.
- Wait 72 hours. If you’ve had grapefruit and need to start a new medication, wait three full days before taking it.
- Switch if needed. Many alternatives exist. For example, switching from simvastatin to rosuvastatin removes the risk entirely. Over 14,000 patients have been switched to safer options through pharmacist-led programs since 2020.
Even if you’ve been drinking grapefruit juice with your meds for years without issues, that doesn’t mean it’s safe. The effect can build up over time. One day, your body might react differently-especially if you get sick, start a new drug, or your liver function changes.

What’s Being Done About It?
The medical community is waking up. Electronic health records now include over 128 automated alerts for grapefruit interactions. Drug interaction software flags grapefruit as one of the top 18% of food-drug risks.
Some drugmakers are responding. The extended-release version of felodipine causes a smaller spike in blood levels than the regular kind. Researchers are even working on gene-edited grapefruit that lack furanocoumarins-still in trials, but promising.
Still, the safest rule hasn’t changed: if your medication is on the list, skip grapefruit entirely. No exceptions. No "just a little." No "I’ve never had a problem before." The science is clear: the risk isn’t theoretical. It’s documented in hospitals, in death reports, and in clinical studies.
The European Medicines Agency recorded 12 deaths linked to grapefruit-drug interactions between 2000 and 2019. In the U.S., over 85 serious adverse events are reported each year. These aren’t rare accidents. They’re preventable.
Final Thought: Your Meds Are Precise. Your Juice Isn’t.
Doctors prescribe exact doses because they’re calibrated for safety and effectiveness. Grapefruit juice throws that precision out the window. It doesn’t matter if you drink it with breakfast, lunch, or dinner. Once it hits your gut, it starts blocking enzymes-and you won’t feel a thing until it’s too late.
There’s no such thing as a "safe amount" when it comes to high-risk medications. The only reliable choice is complete avoidance.
If you’re unsure whether your medication is affected, don’t guess. Call your pharmacy. Check the label. Or ask your doctor for a simple alternative. Your body doesn’t need grapefruit juice to be healthy. But it absolutely needs your medication to work as intended.
Can I drink grapefruit juice if I take my medication at night?
No. Grapefruit juice damages intestinal enzymes that take about 72 hours to recover. Even if you take your pill at night and drink juice in the morning, the enzyme inhibition is still active. The timing doesn’t matter-only the presence of grapefruit within three days of taking the drug.
Is grapefruit juice safe with over-the-counter drugs?
Some are. But many aren’t. For example, the allergy medication fexofenadine (Allegra) is affected because grapefruit blocks its absorption. Other OTC painkillers like ibuprofen or acetaminophen are generally safe. Always check the label or ask a pharmacist-don’t assume OTC means safe with grapefruit.
Does cooking or heating grapefruit destroy the harmful compounds?
No. Furanocoumarins are heat-stable. Whether you eat the fruit raw, blend it into a smoothie, or bake it into a dessert, the chemicals remain active. Marmalade made from Seville oranges is just as dangerous as fresh grapefruit juice.
Can I switch to orange juice instead?
Yes. Regular sweet oranges (like navel or Valencia) and tangerines do not contain furanocoumarins and are safe to consume with medications. Avoid Seville oranges, pomelos, and limes if you’re unsure-stick to standard orange juice.
Why don’t all doctors warn patients about this?
Many do, but the warning isn’t always communicated clearly. A 2021 study found only 37% of pharmacists consistently counsel patients on grapefruit risks. Some doctors assume patients will read labels, or they’re unaware of newer interactions. If you’re on medication, it’s your responsibility to ask-don’t wait for them to bring it up.
Are there any benefits to grapefruit juice interactions?
Researchers are exploring whether the mechanism could be used intentionally-for example, to boost absorption of certain cancer drugs or monoclonal antibodies. But these are still experimental. For patients, there are no proven benefits. The risks far outweigh any theoretical upside.
Nancy Kou
December 21, 2025 AT 02:32This is one of those posts that should be mandatory reading for anyone on prescription meds. I’ve seen too many older relatives ignore warnings until they end up in the ER. Grapefruit isn’t the enemy-it’s the silent saboteur.
Don’t assume your doctor told you. Don’t assume the label says it. Ask. Again. And again.
Knowledge isn’t power here-it’s survival.
Hussien SLeiman
December 22, 2025 AT 21:47Oh, so now we’re blaming citrus for the pharmaceutical industry’s failure to design safer drugs? Fascinating. Let’s not forget that the real issue is lazy prescribing and the fact that 80% of these warnings are buried in 50-page PDFs no one reads. If your drug can’t handle a glass of juice, maybe it shouldn’t be on the market. I’ve been drinking grapefruit with my statin for 12 years. No rhabdomyolysis. No hospital visits. Just a guy who reads the fine print and still chooses flavor over fear.
Also, did you know that 37% of Americans can’t find their own pancreas on a diagram? Maybe we should start there.
Guillaume VanderEst
December 24, 2025 AT 17:21I used to drink grapefruit juice every morning with my blood pressure med. Then one day I passed out in the grocery store. Not because I drank too much. Not because I was sick. Just because the juice and the pill had a silent war in my gut.
Turns out, I was lucky. My pharmacist flagged it after I mentioned the dizziness. Switched to oranges. No more fainting. No more panic.
It’s not about being paranoid. It’s about being alive.
Also, pomelo marmalade? Yeah, I didn’t know that either. Now I know. Thanks, internet.
Alisa Silvia Bila
December 26, 2025 AT 10:00Thank you for this. So clear. So necessary.
I’m on cyclosporine after my transplant. I used to love grapefruit. Now I just drink orange juice. No regrets.
Janelle Moore
December 26, 2025 AT 20:09Wait… so this is all a Big Pharma plot? They know grapefruit blocks the enzyme so they can sell you more expensive drugs? That’s why they don’t warn you-they WANT you to get sick so you’ll switch to their new version! And the FDA? They’re in on it. Look at how many people die every year from grapefruit. It’s not an accident. It’s a profit motive. I’ve got my 5G detector and my aluminum foil hat ready. Don’t drink the juice. Don’t trust the label. Don’t trust the doctor. Trust your gut. And your gut says: THEY’RE LYING TO YOU.
Henry Marcus
December 28, 2025 AT 04:20GRAPEFRUIT JUICE IS A BIOLOGICAL WEAPON DESIGNED BY BIG PHARMA TO CONTROL THE ELDERLY!!!
THEY KNOW CYP3A4 IS THE GATEKEEPER-AND THEY’RE USING CITRUS TO MAKE US DEPENDENT ON THEIR $$$ DRUGS!!!
EVERY TIME YOU DRINK IT, YOU’RE PAYING FOR A NEW PRESCRIPTION!!!
THEY EVEN PUT IT IN THE LABELS SO YOU THINK YOU’RE BEING WARNED-BUT IT’S A TRAP!!!
THEY’RE USING FURANOCOUMARINS TO SLOW DOWN YOUR METABOLISM SO YOU’LL NEED MORE MEDS!!!
AND DON’T EVEN GET ME STARTED ON THE ORANGE JUICE-IT’S A DISTRACTION!!!
THEY’RE USING VITAMIN C TO MASK THE REAL TOXINS!!!
IT’S ALL CONNECTED!!!
THEY’RE HIDING THE TRUTH IN THE FDA DATABASE!!!
THEY KNOW WHAT THEY’RE DOING!!!
THEY’RE NOT DOING IT FOR HEALTH-THEY’RE DOING IT FOR PROFITS!!!
WHY DO YOU THINK THEY DON’T BAN GRAPEFRUIT?!
BECAUSE THEY OWN THE FARMS!!!
IT’S A CONSPIRACY!!!
AND YOU’RE PART OF IT!!!
Carolyn Benson
December 28, 2025 AT 19:03It’s not about grapefruit. It’s about the illusion of control. We think we’re making choices-taking pills, drinking juice, managing health. But we’re just variables in a biochemical equation we don’t understand.
The enzyme doesn’t care if you’re 25 or 75. It doesn’t care if you’re ‘responsible.’ It just does its job-until it doesn’t.
And then you’re just another statistic in a hospital bed, wondering why your body betrayed you.
Science didn’t fail you. You failed to acknowledge how little you actually control.
It’s not about avoiding juice. It’s about accepting your fragility.
That’s the real lesson here.
Chris porto
December 30, 2025 AT 05:50My dad took simvastatin for 10 years and drank grapefruit juice every day. He never had an issue. Then he switched to rosuvastatin after his pharmacist asked him. He said, ‘Why didn’t anyone tell me this before?’
That’s the problem-not the juice. Not the science. The communication.
We assume everyone knows. But they don’t.
So if you’re reading this, and you’re on meds-ask your pharmacist. Just ask.
It takes 30 seconds. Could save your life.
Simple. But nobody does it.
So here I am, doing it for you.
William Liu
December 31, 2025 AT 12:15Good post. Really well-researched.
Just wanted to say-switching to orange juice doesn’t mean giving up flavor. It means keeping your life. And that’s worth more than any citrus tang.
Stay safe out there.
Aadil Munshi
January 1, 2026 AT 01:53Interesting how everyone here treats this like a medical issue. Let’s zoom out. Why are we so dependent on synthetic drugs that a single fruit can break them? Why don’t we fix the root problem-our broken metabolic systems? Why not heal instead of replace? Grapefruit isn’t the villain. Our pharmaceutical dependency is.
Also, I’ve seen people in India take grapefruit with statins for decades. No issues. Maybe it’s the soil? Maybe it’s genetics? Maybe we’re overmedicating? Just saying-let’s not turn a biochemical quirk into a moral panic.
Still, if you’re on cyclosporine? Don’t risk it. I’m not saying don’t worry-I’m saying think deeper.
Erica Vest
January 1, 2026 AT 12:12Correction: The FDA lists 87 medications with known grapefruit interactions as of 2024, not 85. The number has increased slightly due to new data on antivirals and anticoagulants. Also, the 330% increase in simvastatin levels was observed in a 2012 study with 200 mL of juice-actual variability ranges from 150% to 500% depending on individual enzyme expression. Source: FDA Drug Safety Communication, 2024 Update. Always verify with current labeling and your pharmacist. This post is otherwise accurate and well-structured.
Kinnaird Lynsey
January 2, 2026 AT 13:45I appreciate the depth here. But I also want to acknowledge how scary this is for people who don’t have easy access to pharmacists or healthcare. Not everyone can just ‘switch meds’ or ‘ask their doctor.’
It’s a privilege to have options.
Maybe the real issue isn’t just grapefruit.
It’s that our system makes it so hard to stay safe.
Glen Arreglo
January 3, 2026 AT 14:56As someone who grew up in a household where grapefruit juice was a daily ritual, I didn’t know any of this until I moved to the US and got prescribed a calcium channel blocker. My Canadian mom would’ve been horrified.
But here’s the thing-this isn’t just a medical issue. It’s a cultural one. In the US, we treat medicine like candy. In other places, people still respect the body’s balance.
Maybe we need to stop treating drugs like magic bullets and start treating our bodies like ecosystems.
Also, oranges are delicious. Try them.
shivam seo
January 4, 2026 AT 09:45Wow. So now we’re telling people they can’t drink grapefruit juice because some American drug company can’t make a stable molecule? Pathetic. In Australia, we just take our meds and drink what we want. If your body can’t handle a little citrus, maybe you shouldn’t be on pills at all. This is overmedicalization at its finest. Who needs health when you’ve got fear?