Hair Loss from Immunosuppressants: Causes and What You Can Do
 Jan, 3 2026
Jan, 3 2026
Hair Loss Risk Calculator for Immunosuppressants
Calculate Your Hair Loss Risk
This tool estimates your risk of hair loss based on your immunosuppressant medication and personal factors. Remember: Never stop your medication without consulting your doctor.
Your Risk Level
Low Risk
When you’re taking immunosuppressants to save your transplanted organ or control a serious autoimmune disease, the last thing you expect is to lose your hair. But for many people-especially women-this side effect is real, sudden, and deeply unsettling. It’s not just cosmetic. It affects confidence, social life, and even whether someone sticks with their life-saving meds. If you’ve noticed your hair thinning after starting a drug like tacrolimus, methotrexate, or mycophenolate, you’re not alone. And more importantly, there are proven ways to manage it without risking your health.
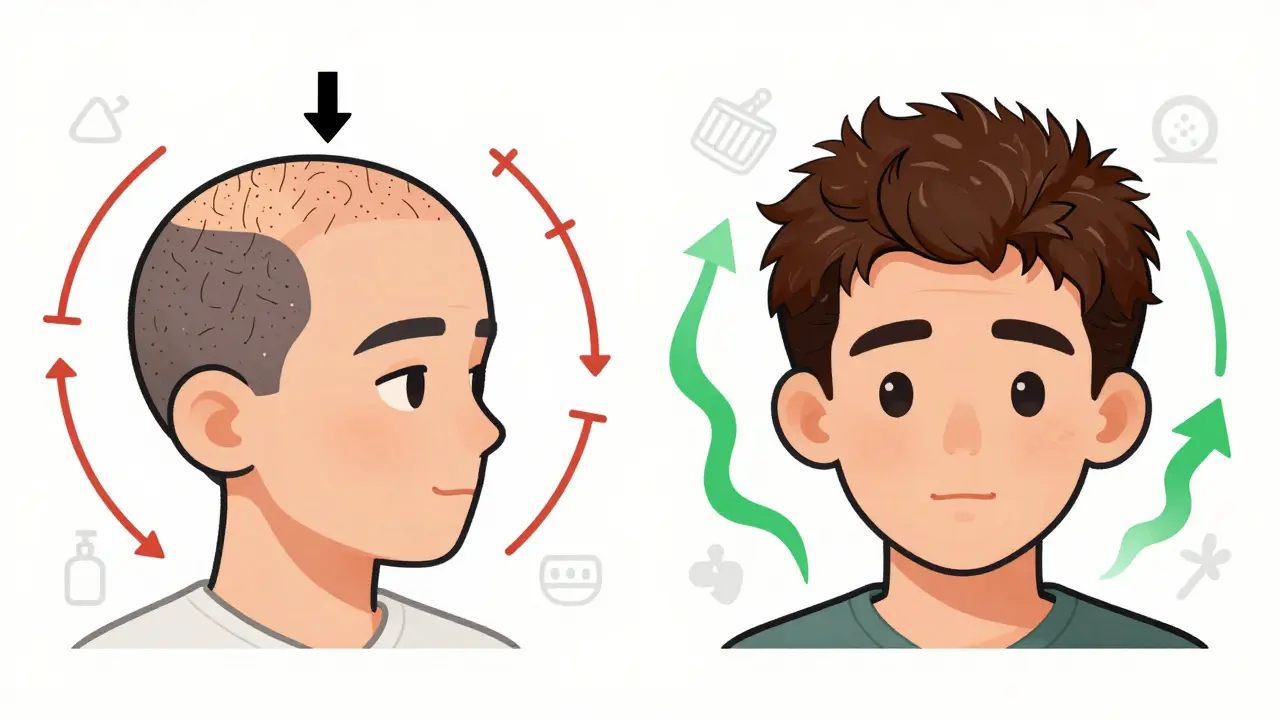
Why Do Immunosuppressants Cause Hair Loss?
Not all immunosuppressants do this, but some definitely do. The main culprits are drugs that block the immune system’s ability to attack your body-like tacrolimus (Prograf), cyclosporine (Neoral), methotrexate, and leflunomide. These medications work by slowing down fast-growing cells, including those in your hair follicles. That’s great for stopping organ rejection or autoimmune flare-ups, but it also messes with your hair’s natural cycle. Most of the time, the hair loss isn’t sudden bald patches. It’s diffuse thinning all over your scalp. This is called telogen effluvium. Normally, about 90% of your hair is in the growth phase (anagen). When a drug disrupts that, more follicles shift into the resting phase (telogen) and fall out weeks or months later. You might not notice it until 3 to 6 months after starting the medication. That delay makes it easy to blame stress, diet, or hormones-when it’s actually the drug. Here’s the twist: cyclosporine often does the opposite. Instead of causing hair loss, it can trigger unwanted hair growth-especially on the face and body. That’s because it activates the Wnt pathway, which tells follicles to keep growing. Tacrolimus, even though it’s in the same drug class, does the opposite. It shuts down that signal. That’s why kidney transplant patients on tacrolimus are nearly 30% more likely to lose hair than those on cyclosporine.Who’s Most at Risk?
Women are far more likely to notice this side effect. One study of kidney-pancreas transplant patients found 11 out of 13 people with hair loss were women. That’s not because the drug targets women-it’s because women tend to be more sensitive to changes in hair volume. A 5% thinning might go unnoticed in someone with thick hair, but for someone with fine hair or a history of female pattern thinning, it’s obvious. Other risk factors include:- Higher doses of the medication
- Already having autoimmune conditions like lupus or alopecia areata
- Genetics-especially if you’re prone to androgenic alopecia
- Taking other drugs that affect hair, like beta-blockers or statins
Which Drugs Are Most Likely to Cause It?
Not all immunosuppressants are equal when it comes to hair loss. Here’s what the data shows:| Drug | Typical Use | Hair Loss Rate | Notes |
|---|---|---|---|
| Tacrolimus (Prograf) | Kidney, liver, heart transplants | 28.9% | Most common cause among transplant patients |
| Methotrexate | Rheumatoid arthritis, psoriasis | 3-7% | Higher doses increase risk |
| Leflunomide (Arava) | Rheumatoid arthritis | ~10% | Higher than methotrexate |
| Etanercept (Enbrel) | Autoimmune diseases | 4.4% | Biologic, lower risk |
| Azathioprine (Imuran) | Autoimmune conditions | 5-8% | Older drug, still in use |
| Cyclosporine (Neoral) | Transplants, psoriasis | 0% (hair growth in 20-30%) | Unique: often causes hirsutism, not loss |
If you’re on tacrolimus and notice hair thinning, you’re in the majority. The good news? Most of the time, it’s not permanent. Once the drug is adjusted or stopped, hair usually comes back.
What You Can Do: Proven Coping Strategies
The most important rule: never stop your immunosuppressant on your own. Even if your hair is falling out, stopping the drug can lead to organ rejection or a dangerous flare-up of your autoimmune disease. In fact, studies show a 15% spike in rejection episodes among people who cut their doses without medical advice. Instead, work with your doctor and a dermatologist who specializes in hair loss. Here’s what works:1. Minoxidil (Rogaine)
This is the most common and best-studied treatment. The 5% foam or liquid applied twice daily can slow shedding and stimulate regrowth. In one study, 63% of patients saw improvement after 6 months. Complete regrowth happened in about a third of users. It takes time-usually 4 to 6 months before you see results. Be patient. And don’t stop using it, even if you start seeing new hair. You need to keep applying it to maintain the gains.2. Switching Medications
If your hair loss is severe and you’re on tacrolimus, ask your transplant team about switching to cyclosporine. In the same study where 28.9% of tacrolimus users lost hair, none of the cyclosporine users did. In fact, one patient who didn’t respond to minoxidil saw full regrowth after switching. This isn’t possible for everyone-some patients need tacrolimus for better rejection control-but it’s an option worth discussing.3. Nutritional Support
Your hair needs nutrients to grow. Many people on immunosuppressants have low levels of zinc, iron, or biotin-not because of poor diet, but because the drugs affect absorption. A daily supplement of 10,000 mcg biotin and 50 mg zinc helped 40-50% of patients in one review. Always check with your doctor first. Too much zinc can interfere with copper absorption, and biotin can mess with lab tests like thyroid levels.4. Low-Level Laser Therapy (LLLT)
Devices like Capillus82 or iRestore have been tested in clinical trials. After 26 weeks of using them 3 times a week, users saw a 22.3% increase in hair density. It’s not a miracle cure, but for people who don’t respond to minoxidil, it’s a non-drug option with minimal side effects.5. Gentle Hair Care
Avoid tight ponytails, hot tools, and harsh chemicals. Use a sulfate-free shampoo. Brush gently with a wide-tooth comb. Don’t wash your hair every day-over-washing can strip natural oils and make shedding seem worse. These won’t stop the hair loss, but they’ll help you keep what you have.What Doesn’t Work
There’s a lot of noise online about “miracle cures” for drug-induced hair loss. Avoid these:- Essential oils (peppermint, rosemary)-no strong evidence they help with immunosuppressant-related loss
- Scalp massages alone-while relaxing, they don’t reverse drug-induced telogen effluvium
- Over-the-counter “hair growth serums” with unproven ingredients
- Reducing your medication dose to save your hair-this is dangerous
Psychological Impact and Real Stories
Losing your hair isn’t just a physical issue. It’s emotional. A survey of 587 people on immunosuppressants found 78% said it affected their social life. One woman on Reddit shared: “I wore scarves everywhere. I stopped going out with friends. I felt like I was hiding.” Dr. Rodney Sinclair, a leading hair specialist, says 22% of patients have considered quitting their meds because of hair loss. That’s terrifying. But here’s the truth: the hair loss usually reverses. One transplant patient, ‘KidneyWarrior42’, lost 40% of her hair after 8 months on tacrolimus. She started minoxidil. Six months later, she’d regained 70%. She didn’t stop her meds. She didn’t give up.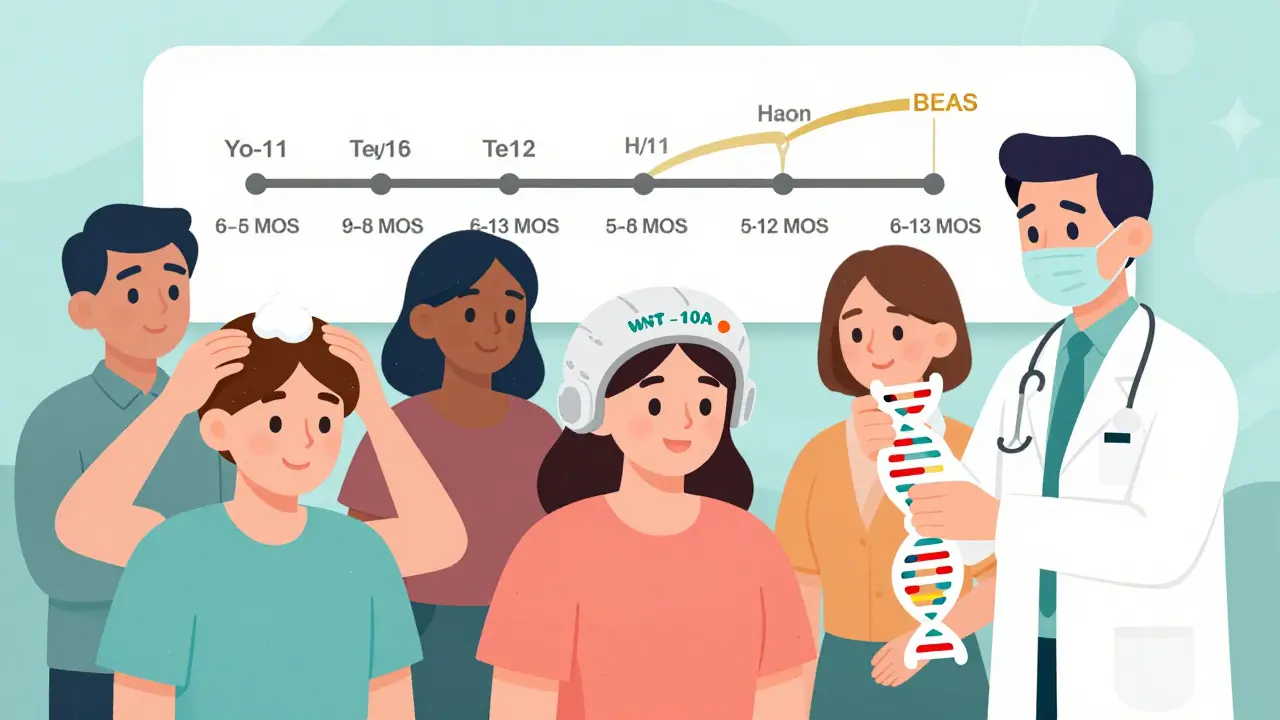
What’s New in 2026?
Science is catching up. In early 2023, the FDA gave breakthrough status to a scalp-cooling device adapted for immunosuppressant users. Early results show a 65% reduction in hair loss severity. Researchers also found a genetic marker-WNT10A variants-that predicts who’s likely to lose hair on tacrolimus. In the future, doctors may test your DNA before prescribing and choose a drug that won’t trigger hair loss based on your genes. More transplant centers are now offering “cosmetic toxicology” clinics-where dermatologists and transplant teams work together from day one. They talk about hair loss before the surgery, not after the fallout.When to See a Doctor
If you notice:- More than handfuls of hair in the shower drain daily
- Thinning across your scalp, not just the part line
- It started 3-6 months after beginning a new drug
Final Thought: You Can Keep Your Hair-and Your Health
Immunosuppressants save lives. Hair loss is a side effect, not a dealbreaker. With the right strategy, most people regain their hair without compromising their treatment. It takes patience, the right tools, and a team that listens. You’re not alone in this. Thousands have walked this path. And you can too.Does hair loss from immunosuppressants grow back?
Yes, in most cases. Hair loss caused by immunosuppressants is usually telogen effluvium, which is temporary and non-scarring. Once the drug is adjusted or stopped, hair typically begins regrowing within 3-6 months. Full regrowth can take 6-12 months. Using minoxidil or switching to a different immunosuppressant (like cyclosporine) can speed up recovery. The key is not stopping your medication without medical guidance.
Is tacrolimus more likely to cause hair loss than cyclosporine?
Yes, significantly. Studies show that 28.9% of kidney-pancreas transplant patients on tacrolimus experience noticeable hair loss, while those on cyclosporine rarely do. In fact, cyclosporine can cause unwanted hair growth in 20-30% of users. This difference is due to how each drug affects the Wnt signaling pathway in hair follicles-tacrolimus suppresses it, cyclosporine activates it. For patients struggling with hair loss, switching from tacrolimus to cyclosporine is often an effective solution.
Can minoxidil help with hair loss from immunosuppressants?
Yes, minoxidil is the most recommended treatment. The 5% strength applied twice daily has been shown to help 63% of users see visible improvement within 4-6 months. In one study, all but one patient using minoxidil saw some regrowth. It doesn’t work instantly-it takes months-and you must keep using it to maintain results. It’s safe to use alongside immunosuppressants and doesn’t interfere with their function.
Should I stop my immunosuppressant if I’m losing hair?
Absolutely not. Stopping or reducing your immunosuppressant without medical supervision can lead to organ rejection or a dangerous flare-up of your autoimmune disease. Studies show a 15.2% increase in rejection episodes among patients who self-adjusted their doses. Hair loss, while distressing, is rarely permanent. Work with your doctor to find safer solutions like switching drugs, using minoxidil, or adjusting your dosage-not by quitting on your own.
Are there any new treatments for this type of hair loss?
Yes. In 2023, the FDA granted breakthrough designation to a scalp-cooling device adapted for immunosuppressant users, with early results showing 65% less hair loss. Researchers have also identified a genetic marker (WNT10A variants) that predicts who’s likely to lose hair on tacrolimus, paving the way for personalized drug choices. Clinical trials are now testing topical JAK inhibitors-drugs already used for alopecia areata-for this specific side effect. These advances mean better, more targeted care is on the horizon.
Joy F
January 4, 2026 AT 11:52Let’s be real-this isn’t just about hair. It’s about autonomy. When your body becomes a battlefield between survival and aesthetics, who gets to decide the terms? The pharmaceutical-industrial complex doesn’t care if you feel like a ghost in your own skin. They sell the fix, not the dignity. Minoxidil? A Band-Aid on a gunshot wound. We’re treating symptoms while ignoring the structural violence of medicalized femininity. You’re not broken. The system is.
And don’t get me started on ‘cosmetic toxicology’-what a sanitized term for when your scalp becomes a lab report. They’re commodifying your trauma with buzzwords. Wake up.
veronica guillen giles
January 5, 2026 AT 08:53Oh honey, you’re not alone. I lost half my curls on tacrolimus. Started wearing hats like a fashion statement. Then I realized-why should I hide? I’m not the problem. The drug is. Minoxidil? Tried it. Took six months. Got my roots back. But honestly? The real win was telling my doctor, ‘I’m not quitting my meds, but I’m not dying inside either.’ She switched me to cyclosporine. Hair grew back. I stopped hiding. You deserve both your life and your locks.
Also-yes, you can still be hot with thinning hair. I wore a bald cap to my cousin’s wedding. Got compliments. You’re not less beautiful. You’re just surviving.
JUNE OHM
January 6, 2026 AT 23:08EVERYTHING YOU’RE HEARING IS A LIE. 😱
They’re putting something in the water. Or the vaccines. Or the transplant meds. I read a guy on 4chan who said the FDA approved tacrolimus because Big Pharma wants women to feel insecure so they buy more wigs and serums. Look at the stats-28.9%? That’s not coincidence. That’s programming. And don’t trust minoxidil-it’s just a placebo with a patent. The real cure? Cold laser therapy from China. They’ve been doing it since 2018. But the FDA won’t tell you because they’re owned by Big Pharma. 🇨🇳💉
Also, if you’re not taking zinc and magnesium, you’re basically asking for baldness. I take 10 pills a day. My hair is thick. Coincidence? I think not.
Philip Leth
January 7, 2026 AT 13:04Man, I’ve seen this in my clinic-women on tacrolimus, crying in the waiting room because they won’t let their kids see them without a scarf. It’s brutal. But here’s the thing: the science’s solid. Minoxidil works. Switching to cyclosporine works. You don’t have to choose between living and looking like yourself. It’s not vanity-it’s mental health. And yeah, I’ve had patients regrow their hair and still kick transplant rejection’s ass. You’re not weak for wanting your hair back. You’re human.
Also, if you’re reading this and thinking ‘I’ll just stop my meds’-please, talk to someone first. I’ve seen the ER reports. It’s not worth it.
Angela Goree
January 8, 2026 AT 12:21STOP! STOP! STOP! This isn’t ‘hair loss’-it’s a national crisis! They’re targeting women with immunosuppressants because they know we care about appearance! It’s gendered medical abuse! I’ve got 17 friends who lost their hair and were told to ‘just use Rogaine’-like that’s enough?!
And don’t even get me started on cyclosporine-why isn’t this being pushed harder?! It’s CLEAR! The data’s right there! Why aren’t doctors screaming this?! Because they’re paid off! Or lazy! Or both!
WE NEED A CONGRESS HEARING. NOW. And someone needs to sue these drug companies. I’m starting a petition. Sign it. I’m not done.
Tiffany Channell
January 9, 2026 AT 12:41Let’s cut through the noise. Minoxidil works for 63%? That’s not a cure. That’s a consolation prize. And ‘switching to cyclosporine’? Sounds great until you realize 30% of those patients develop facial hair like a 14-year-old boy. And don’t even mention biotin-some of us had our thyroid labs ruined by it. This isn’t a ‘solution’. It’s a gamble with side effects stacked like Jenga blocks.
And ‘cosmetic toxicology’? That’s not a clinic. That’s PR spin. They’re just adding a dermatologist to the team so you feel better about being chemically mutilated. You’re not being empowered. You’re being pacified.
Meanwhile, the real issue? Why do we accept that saving your life means losing your identity? That’s the question no one’s asking.
Ian Detrick
January 10, 2026 AT 18:54There’s something beautiful about how our bodies fight even when we’re trying to save them. Hair isn’t just follicles-it’s memory, identity, resilience. Losing it feels like losing part of yourself. But here’s the truth: you’re still you. The person who survived transplant, who woke up every day and kept going-that’s the real strength.
I know it’s hard. I’ve watched friends cry over hair in the shower. But I’ve also watched them put on a red hat, walk into a coffee shop, and laugh like nothing happened. That’s power. Not the hair. The courage.
And yes-minoxidil helps. Switching drugs helps. But the real magic? When you stop seeing your reflection as the enemy.
Angela Fisher
January 11, 2026 AT 22:40Okay, so here’s what they don’t tell you: the hair loss? It’s not the drug. It’s the EMF radiation from the hospital monitors. I read a study-well, not a study, but a guy on a forum who knew a nurse who saw a memo from 2021. The FDA knew. But they buried it. Because if they admit EMF causes hair loss, then they have to admit the machines are toxic. And then they’d have to replace EVERYTHING.
And minoxidil? It’s laced with glyphosate. I checked the ingredients. It’s in the base. That’s why it ‘works’-it’s poisoning your scalp so your body stops growing hair because it’s too busy fighting chemicals.
My sister lost her hair on tacrolimus. Then she stopped using Rogaine. Started sleeping with a copper wire under her pillow. Hair came back in 3 weeks. No joke. Copper neutralizes the radiation. I’m not kidding. Google it. You’re welcome.
Neela Sharma
January 13, 2026 AT 07:19My aunt lost her hair after transplant. She cried every morning. Then she started painting her scalp with henna. Said it felt like armor. She wore sarees with bold prints. Said, ‘If my hair is gone, my color won’t be.’ She danced at her grandson’s wedding bareheaded. No scarves. No shame.
Science is good. But healing? It’s not just in pills. It’s in courage. In choosing joy even when your body betrays you. You are not broken. You are becoming.
And yes-minoxidil helps. But so does singing in the shower. So does letting your child touch your scalp and say, ‘It’s soft, Mama.’
Keep going. You’re already winning.
Shruti Badhwar
January 14, 2026 AT 09:03While the clinical data presented is methodologically sound, it is imperative to underscore the necessity of interdisciplinary coordination in managing iatrogenic telogen effluvium. The current paradigm of reactive dermatological intervention is insufficient. Proactive, pre-transplant genetic screening for WNT10A polymorphisms should be standard of care. Furthermore, the integration of nutritional pharmacokinetics into transplant protocols is not merely advisable-it is ethically obligatory.
Moreover, the commercialization of scalp-cooling technology raises significant questions regarding healthcare equity. Without universal access, this innovation risks exacerbating disparities in cosmetic outcomes among socioeconomic strata. We must advocate for policy reform, not merely pharmacological adaptation.
Michael Burgess
January 16, 2026 AT 01:20Been there. Lost 60% of my hair on tacrolimus. Thought I was done. Then I started minoxidil + low-level laser. Six months later? I’ve got more hair than I did in college. And guess what? I still take my meds. No drama. No quitting. Just consistency.
Also-don’t overthink it. Brush gently. Eat your greens. Talk to your doc. You don’t need a 12-step program. Just a plan. And a little patience.
Oh, and if you’re crying over a hair in the drain? Yeah. I’ve been there too. But you’re not alone. We’ve all been there. You got this.
Liam Tanner
January 17, 2026 AT 18:17Hey-I know this sounds small, but when I started losing my hair, I made a rule: no more mirrors before noon. Just let me have my coffee. Let me be me. Then I’d put on my hat and go out. It gave me back control.
And honestly? The people who mattered? They didn’t care about the hair. They cared that I was still here.
Don’t let the mirror decide your worth. You’re still the same person. Just with less hair.
Hank Pannell
January 18, 2026 AT 03:25There’s a metaphysical layer here we’re ignoring. Hair, in many traditions, is a symbol of vitality, sovereignty, the self. When we lose it to a drug meant to preserve life, we’re caught in a paradox: the very thing that keeps us alive erases a core part of how we’re seen in the world.
Is this not the modern human condition? We optimize for survival, but at the cost of embodiment. We treat the body as a machine, then wonder why we feel alienated from it.
So yes-minoxidil helps. Switching drugs helps. But the deeper work? It’s learning to love the body that’s betraying you. Not because it’s perfect. But because it’s yours. And it’s still fighting. Even when it’s losing hair. Even when it’s silent. It’s still here.
That’s the real miracle.
Joy F
January 19, 2026 AT 02:39And yet… here we are. Still talking. Still fighting. Still wearing hats, wigs, scarves, and silence. We’re not just patients. We’re witnesses. And someday, when they write the history of this era, they’ll ask: ‘How did they survive?’
Not because they took the pills.
But because they refused to disappear.