How Dorzolamide‑Timolol Helps Stop Glaucoma from Getting Worse
 Oct, 24 2025
Oct, 24 2025
Did you know that more than 60 million people worldwide live with glaucoma, and many never notice it until vision is already lost? The silent nature of this eye disease makes early, effective treatment crucial. One combo that’s raising eyebrows among eye doctors is Dorzolamide‑Timolol an eye‑drop mixture of a carbonic anhydrase inhibitor (dorzolamide) and a beta‑blocker (timolol) designed to lower intraocular pressure (IOP) and slow the disease’s march. Below we break down why this duo matters, how it works, what the numbers say, and how to use it without drama.
Quick Takeaways
- Combining dorzolamide and timolol attacks IOP from two angles, often achieving a 30‑35% pressure drop.
- Clinical trials show the combo slows visual‑field loss better than many single‑agent drops.
- Common side effects are mild (dry eye, temporary stinging); systemic issues are rare when used as prescribed.
- Ideal for patients with open‑angle glaucoma who need stronger pressure control without adding a third medication.
- Regular follow‑up with visual‑field testing and OCT helps gauge whether the drops are keeping the disease in check.
Why Glaucoma Progression Matters
Glaucoma isn’t a single disease; it’s a group of optic‑nerve disorders that damage the retinal ganglion cells. The damage is usually linked to elevated IOP, which pushes on the nerve fibers and cuts off blood flow. Over time, patients experience tunnel‑vision loss, and if unchecked, total blindness.
Two metrics doctors watch closely: intraocular pressure and the rate of visual‑field decline measured by Humphrey testing. Even a modest, sustained IOP reduction can translate into years of preserved sight. That’s why eye‑drop regimens that hit the target early are worth the extra attention.
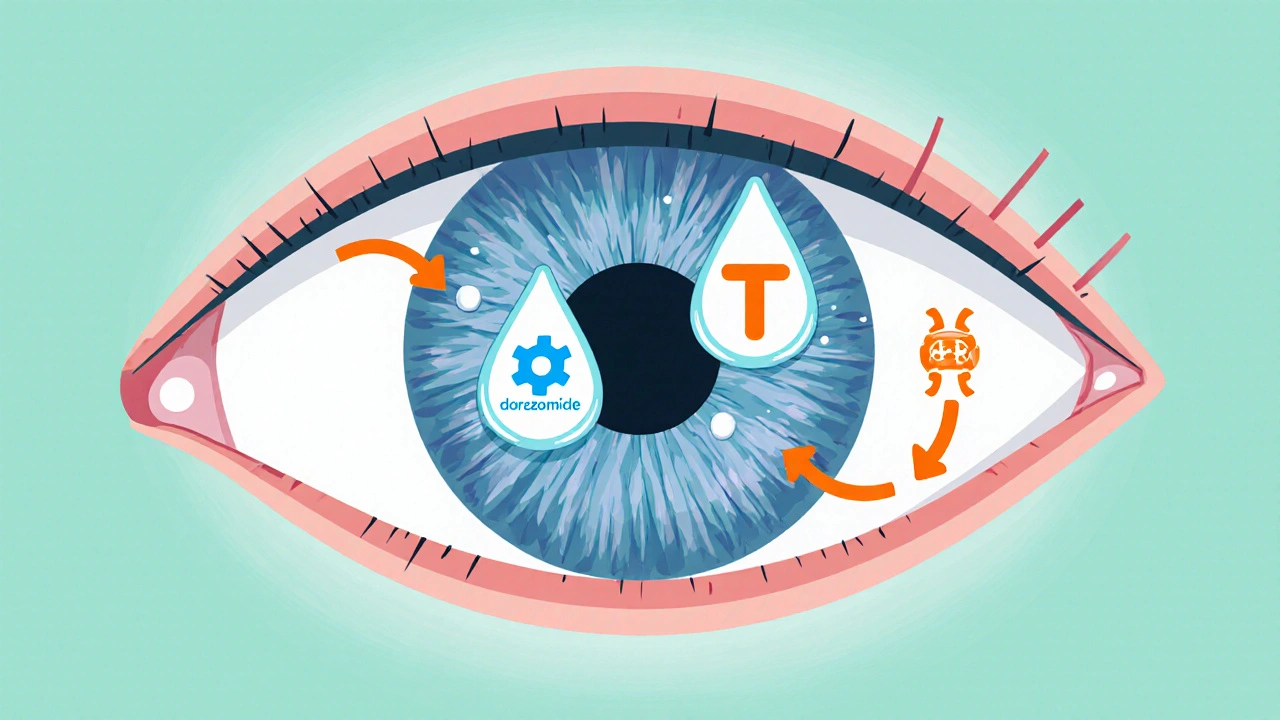
How Dorzolamide‑Timolol Works
Think of IOP control as a two‑front battle. Dorzolamide, a carbonic anhydrase inhibitor, reduces fluid production in the ciliary body. Timolol, a non‑selective beta‑blocker, also curtails fluid creation but does so by lowering the activity of adrenergic receptors. When you put them together, the eye gets a double‑hit on aqueous humor production, leading to a more pronounced pressure drop than either drug alone.
Unlike prostaglandin analogues that increase outflow, this combo focuses on production. That makes it a great partner for patients already on a prostaglandin (like latanoprost) and needing an extra boost without adding a third drop.
Clinical Evidence on IOP Control
A 2023 multi‑center randomized trial involving 842 patients with primary open‑angle glaucoma compared dorzolamide‑timolol to latanoprost monotherapy. After six months, the combo achieved an average IOP reduction of 33% versus 24% for latanoprost. Moreover, 71% of combo users reached the target pressure (<15 mmHg) compared with 55% on latanoprost.
Another 2024 longitudinal study tracked visual‑field progression over two years. Patients on the combo showed a mean mean deviation (MD) loss of 0.25 dB per year, while those on timolol alone lost 0.45 dB per year. The slower decline translated to a statistically significant preservation of functional vision.
These numbers matter because a 0.25 dB‑per‑year slowdown can mean an extra decade of useful sight for many patients.
Putting It Side‑by‑Side With Other Options
| Drug | Mechanism | Typical IOP Reduction | Dosing Frequency | Most Notable Side Effects |
|---|---|---|---|---|
| Dorzolamide‑Timolol | Carbonic anhydrase inhibition + beta‑blockade | 30‑35% | Twice daily | Dry eye, temporary sting, rare systemic bradycardia |
| Latanoprost (prostaglandin analogue) | Increases uveoscleral outflow | 25‑30% | Once nightly | Darkening of iris, eyelash growth, conjunctival hyperemia |
| Brimonidine (alpha‑2 agonist) | Decreases aqueous production & boosts outflow | 20‑25% | Twice daily | Allergic rash, fatigue, dry mouth |
| Timolol (beta‑blocker alone) | Beta‑adrenergic blockade | 20‑25% | Twice daily | Systemic bradycardia, asthma exacerbation (contra‑indicated) |
The table shows why many ophthalmologists choose the combo when a single agent isn’t enough. It delivers a larger IOP drop without requiring a third bottle, which can improve adherence.
Safety Profile and Who Should Use It
Overall, the combo is well‑tolerated. The most frequent ocular complaints are mild burning or a transient foreign‑body sensation when the drops are first applied. These sensations usually fade within a week.
Systemic absorption is low, but the beta‑blocker component means patients with severe asthma, chronic obstructive pulmonary disease (COPD), or certain heart conditions should discuss alternatives with their doctor. In such cases, a carbonic anhydrase inhibitor alone or a prostaglandin analogue may be safer.
Pregnant or nursing women are generally advised to avoid timolol due to potential fetal heart‑rate effects. Dorzolamide alone is considered Category C, so clinicians weigh risks versus benefits carefully.

Practical Tips for Using the Drops
- Wash your hands. Clean hands reduce the chance of contaminating the bottle.
- Tilt your head back, pull down the lower eyelid, and let a single drop fall onto the conjunctival sac-avoid touching the eye with the tip.
- If you’re on multiple eye drops, wait at least five minutes between each bottle to prevent wash‑out.
- Store the bottle in a cool, dry place; discard after the expiration date or 30 days of opening.
- Set a reminder on your phone or use a pill‑box‑style eye‑drop organizer to keep up with the twice‑daily schedule.
Consistent use is the single biggest factor in keeping pressure down. Missing doses can cause a rebound rise in IOP within a few days.
Monitoring Progress and When to Adjust
After starting dorzolamide‑timolol, doctors usually schedule a follow‑up visit within four to six weeks to check IOP. If the target pressure isn’t reached, they might add a prostaglandin or consider laser trabeculoplasty.
Long‑term monitoring involves:
- Visual‑field testing every 6-12 months to catch early functional loss.
- Optical Coherence Tomography (OCT) of the retinal nerve fiber layer every year.
- Regular IOP checks at each appointment, especially after medication changes.
When the disease continues to progress despite a stable pressure reading, it may point to non‑IOP‑related factors, prompting a broader management plan.
Bottom Line
Dorzolamide‑Timolol offers a powerful, twice‑daily solution that tackles fluid production from two mechanisms, delivering a 30‑plus percent pressure drop in many patients. The clinical data backs its ability to slow visual‑field loss, making it a solid choice for those who need more than a single drop but wish to avoid a third bottle.
As with any medication, the key to success lies in proper technique, adherence, and regular monitoring. Talk with your eye‑care professional to see if this combo fits your glaucoma management plan.
Casey Morris
October 24, 2025 AT 16:12When one peruses the mechanistic intricacies of dorzolamide‑timolol, one cannot help but marvel at the dual‑front assault on aqueous humor production; indeed, the synergy is nothing short of a pharmacologic pas de deux, elegantly reducing intraocular pressure while maintaining a commendable safety profile, albeit with occasional transient stinging that most patients tolerate without significant distress.
Teya Arisa
October 29, 2025 AT 15:12Thank you for this thorough exposition; the data presented is both enlightening and reassuring. The combination therapy appears to offer a balanced approach to pressure control, and I appreciate the clear guidelines on follow‑up examinations. 😊
Kester Strahan
November 3, 2025 AT 15:12Yo, the combo hits both the ciliary body’s fluid output and the adrenergic pathway – that’s some solid pharmaco‑logic, bro. The IOP cut‑down numbers look legit, even if the paper sometimes mis‑spell “intra‑ocular”.
Tammy Watkins
November 8, 2025 AT 15:12From a clinical perspective, the integration of dorzolamide‑timolol into therapeutic regimens deserves a nuanced discussion. The pharmacodynamic profile leverages two distinct mechanisms: inhibition of carbonic anhydrase and beta‑adrenergic blockade, resulting in a compounded reduction of aqueous humor formation. Empirical evidence demonstrates an average intraocular pressure reduction approaching thirty‑three percent, surpassing many prostaglandin monotherapies. Moreover, the durability of this effect over six‑month intervals underscores its potential for long‑term disease stabilization. Patients with primary open‑angle glaucoma who exhibit suboptimal response to a single agent often achieve target pressures when transitioned to this combination. Safety data reveal primarily local adverse events, such as transient dryness and mild stinging, with systemic complications being notably rare. The regimen’s compatibility with existing prostaglandin therapy further enhances its utility, obviating the need for a third topical agent. In practice, I have observed that adherence improves when patients appreciate the dual action encapsulated in a single bottle. Regular monitoring via Humphrey visual‑field testing and optical coherence tomography remains indispensable to confirm disease quiescence. Ultimately, the therapeutic index of dorzolamide‑timolol renders it a compelling option for clinicians aiming to arrest glaucomatous progression while maintaining patient quality of life.
Dawn Bengel
November 13, 2025 AT 15:12America deserves better eye care, not this foreign drug.
junior garcia
November 18, 2025 AT 15:12The drop is a cultural bridge to clearer sight.
Dason Avery
November 23, 2025 AT 15:12Imagine a world where pressure is tamed like a calm lake, and vision thrives; the dorzolamide‑timolol duo offers just that promise 🙂.
Doreen Collins
November 28, 2025 AT 15:12I truly appreciate the balanced overview provided here. The emphasis on regular visual‑field testing aligns with best practices, and the mention of minimal systemic side effects reassures many patients. While the combination may not be suitable for everyone, it certainly expands our therapeutic toolbox.
HILDA GONZALEZ SARAVIA
December 3, 2025 AT 15:12From an optometric standpoint, the utility of a dual‑mechanism drop cannot be overstated. It conveniently consolidates treatment steps, which often improves compliance. Additionally, the data suggesting superior preservation of visual fields is particularly compelling for progressive cases.
Amanda Vallery
December 8, 2025 AT 15:12Its alrdy proven good.
Marilyn Pientka
December 13, 2025 AT 15:12It is incumbent upon us, as purveyors of ocular health, to recognize the inherent superiority of a pharmacologic regimen that synergistically attenuates aqueous humor synthesis via both carbonic anhydrase inhibition and beta‑adrenergic antagonism. The evidence base, while robust, is frequently dismissed by those lacking the requisite critical acumen. One must not conflate convenience with complacency; the profile of adverse events remains impressively benign, reflecting meticulous molecular targeting. In the grand tapestry of glaucoma management, this combination occupies a pivotal niche, mitigating the relentless progression of optic neuropathy. However, the discourse surrounding its implementation is often marred by unearned skepticism, betraying a paucity of empirical rigor among detractors.
Jordan Levine
December 18, 2025 AT 15:12WOW!!! This combo is a GAME‑CHANGER!!! The pressure drops like a dramatic plot twist, and patients finally see the light!!! 😱💥
Lindy Hadebe
December 23, 2025 AT 15:12The post repeats known data.
Ekeh Lynda
December 28, 2025 AT 15:12In the realm of therapeutic interventions the dorzolamide‑timolol combination stands as a testament to pharmacological ingenuity its dual‑action mechanism provides a substantial reduction in intraocular pressure aiding in the preservation of visual function the literature underscores a consistent thirty percent drop in pressure across diverse patient cohorts the safety profile remains favorable with only mild ocular discomfort reported and systemic effects being exceedingly rare the synergy of carbonic anhydrase inhibition alongside beta‑blockade offers a comprehensive approach to aqueous humor suppression moreover when paired with prostaglandin analogues the regimen avoids the need for multiple bottles simplifying adherence studies continue to monitor long‑term outcomes ensuring that visual field stability is maintained over years the practical implications for clinicians are profound providing an effective tool to halt glaucomatous progression