How Generics Save Trillions in Healthcare: The Real Cost Impact
 Dec, 7 2025
Dec, 7 2025
For every 10 prescriptions filled in the U.S., nine are for generic drugs. Yet those nine prescriptions cost only about 12% of what the brand-name versions do. That’s not a small difference-it’s a trillion-dollar shift in how America pays for health care.
In 2024 alone, generic and biosimilar medications saved the U.S. healthcare system $467 billion. That’s more than the entire annual budget of the Department of Defense. Over the last decade, those savings have added up to $3.4 trillion. This isn’t theoretical. It’s real money staying in patients’ pockets, reducing insurance premiums, and easing pressure on Medicare and Medicaid.
How Generics Work-And Why They’re So Much Cheaper
Generic drugs aren’t knockoffs. They’re exact copies of brand-name drugs in active ingredients, dosage, safety, strength, and how they work in the body. The only differences? The color, shape, or inactive fillers-and the price. A generic version of a popular blood pressure pill might cost $4 a month instead of $150. That’s not a marketing trick. It’s science and regulation working as designed.
The 1984 Hatch-Waxman Act created the legal pathway for generics. It let drug companies skip expensive clinical trials if they could prove their version matched the original. That cut development time from 10 years to under 2. The result? Competition. When a brand-name drug’s patent expires, multiple generic makers enter the market. Prices drop fast. In some cases, a single generic can slash the cost of a drug by 80% within months.
The Numbers Behind the Savings
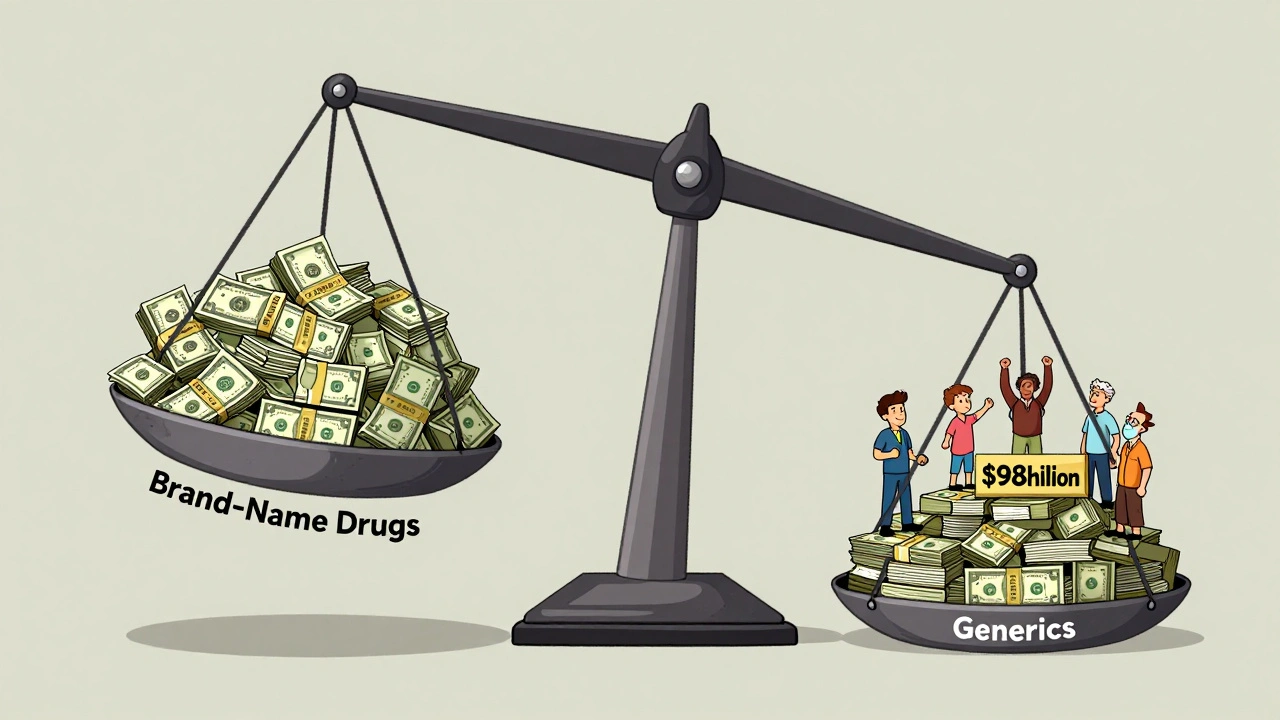
Here’s what the data shows:
- 90.2% of all prescriptions filled in 2024 were for generics-3.9 billion prescriptions.
- Those generics cost only $98 billion total.
- Brand-name drugs? Just 435 million prescriptions-but they cost $700 billion.
That’s a 700% difference in spending for the same treatment. The biggest savings come from drugs used for chronic conditions: high blood pressure, diabetes, high cholesterol, asthma. The top 10 generic drugs saved $89.5 billion in 2023. The top 10 by total savings? $127 billion. That’s not a rounding error. That’s enough to cover free college tuition for millions of students.
Biosimilars-generic versions of complex biologic drugs like Humira or Enbrel-are adding even more. In 2024, they saved $20.2 billion on their own. Since 2015, that number is $56.2 billion. And they’re growing fast. The biosimilar market is expanding at over 22% a year.
Who Benefits the Most?
Patients. Medicare. Medicaid. Employers. Taxpayers.
In 2024, generics saved Medicare $142 billion. Medicaid saved $62.1 billion. That’s not just helpful-it’s essential. Without generics, many seniors would be choosing between their medication and their rent. Medicaid programs, which cover low-income families, would have been overwhelmed.
Even private insurers rely on generics to keep premiums from skyrocketing. Blue Cross Blue Shield estimates that without generics, their members would pay $20 billion more each year just for prescriptions.
And it’s not just the U.S. The average European country uses generics in 60-80% of prescriptions. The U.S. leads the world in adoption. That’s why U.S. patients pay less for the same drugs than people in Germany or France-even though the U.S. spends more overall on healthcare.
Why Aren’t We Saving Even More?
Because the system is being gamed.
Brand-name drugmakers don’t want generics to win. So they use legal tricks to delay them:
- Patent thickets: Filing dozens of minor patents on one drug to block generics. One study found that just four drugs cost the system over $3.5 billion in lost savings over two years.
- Pay-for-delay: Brand companies pay generic makers to stay off the market. These deals cost $12 billion a year, with $3 billion hitting federal programs.
- Product hopping: Switching patients to a slightly modified version of a drug just before the patent expires, resetting the clock.
Then there are pharmacy benefit managers (PBMs). They’re supposed to negotiate lower prices. But many push patients toward brand-name drugs because they get bigger rebates from manufacturers-even when generics are cheaper and just as effective.
Administrative barriers make it worse. Prior authorization requirements for generics rose 47% between 2019 and 2023. Some insurers still make patients jump through hoops to get a $5 pill instead of a $150 one.
Real People, Real Savings
On Reddit, a patient shared how switching from a $800 brand-name drug to a $10 generic changed their life. They could finally afford to fill the prescription every month. That story isn’t rare.
A Drugs.com analysis of over 15,000 reviews found that 87% of users rated the cost of generics as excellent or good. But only 63% said they felt the generic worked as well as the brand. That gap isn’t about science-it’s about perception. Some patients remember the old days when generics had inconsistent quality. Today’s generics are held to the same FDA standards as brand drugs.
Still, a 2023 survey of 500 patients found that 42% had skipped a prescription because of cost. But 89% of those who switched to generics said they were satisfied with both the price and how the drug worked. The average monthly savings? $147 per medication.

What’s Next?
The FDA approved over 1,100 new generic drugs in 2024. Another $24 billion in drug spending is expected to become generic by 2025. That includes complex treatments like injectables and inhalers-drugs that used to cost thousands a month.
Legislation like the Affordable Prescriptions for Patients Act, passed by the Senate HELP Committee in 2024, aims to stop patent abuse and could save $7.2 billion a year. But without enforcement, these laws won’t matter.
There are still risks. Drug shortages affected 287 generic medications in December 2024. Manufacturing is becoming more concentrated-just 10 companies now control 63% of the generic market. That reduces competition and can lead to price spikes.
But the trend is clear. If current policies hold, generics and biosimilars will save $5.1 trillion between 2025 and 2034. That’s more than the entire GDP of Canada.
The Bottom Line
Generics aren’t just a cost-cutting tool. They’re the backbone of affordable healthcare in America. Without them, millions would go without treatment. Insurance companies would collapse under the weight of drug prices. Medicare would be insolvent.
The system works-when it’s allowed to work. The problem isn’t the generics. It’s the barriers keeping them from reaching patients faster. Fix those, and the next trillion-dollar savings isn’t a dream. It’s the next year’s report.
Arun Kumar Raut
December 8, 2025 AT 01:20Generics are the quiet heroes of healthcare. I grew up in India where generics are the only option for most people, and I’ve seen how they let families keep their health without going broke. It’s not magic-it’s just fairness.
When my uncle needed insulin, the brand was $400 a month. The generic? $12. He lived 10 more years because of that difference. No hype, no ads, just science and access.
People who say generics don’t work haven’t lived it. The FDA doesn’t mess around. Same active ingredient, same results. The only thing different is the price tag-and that’s the real win.
precious amzy
December 8, 2025 AT 06:00One must question the epistemological foundations of this discourse. The very notion that ‘savings’ equate to ‘value’ presumes a utilitarian framework that ignores the ontological erosion of pharmaceutical innovation. The commodification of biological equivalence reduces medicine to a transactional calculus-where human health becomes a line item on a balance sheet.
Moreover, the assumption that ‘generic’ implies ‘identical’ is a fallacy of equivalence. Bioavailability variance, even within FDA tolerances, may yield differential therapeutic outcomes across pharmacogenomic subpopulations. One cannot dismiss the subtle phenomenological experience of patient perception as mere ‘myth.’
Carina M
December 9, 2025 AT 15:36How dare you glorify generics as some moral triumph? This is not about saving money-it’s about diluting the sanctity of medical advancement. Brand-name drugs represent decades of research, sacrifice, and intellectual labor. To reduce them to a price tag is not just naive-it’s obscene.
And don’t get me started on the FDA. Their standards are a joke compared to European regulatory rigor. You think $4 pills are safe? You’re just lucky no one died yet. This is the cost of American greed masquerading as efficiency.
William Umstattd
December 10, 2025 AT 02:42Let me be perfectly clear: the systemic sabotage of generic drug access is not an accident-it’s corporate malfeasance. Patent thickets? Pay-for-delay? Product hopping? These are not loopholes. They are crimes.
And pharmacy benefit managers? They’re not intermediaries-they’re parasites. They profit from confusion. They get paid to steer patients toward expensive drugs-even when the cheaper, identical alternative is right there.
Every time someone skips a dose because they can’t afford a $150 pill when a $5 generic exists, it’s not a tragedy. It’s a policy failure. And the people responsible? They’re in boardrooms. Not in labs. Not in clinics. In boardrooms.
We need criminal charges. Not reforms. Charges.
Angela R. Cartes
December 11, 2025 AT 22:46ok but like... why are we even talking about this? 🤡
generics are cheap, brands are expensive, pbms are shady, and i just want my blood pressure pill to not cost my rent. that’s it. 🙃
Andrea Beilstein
December 12, 2025 AT 07:09Generics are the quiet revolution nobody talks about in TED talks or on CNN
They dont have flashy ads or celebrity endorsements but they keep the elderly breathing and the young working
Its not about capitalism or innovation its about dignity
When you can choose between medicine and food its not a market failure its a moral collapse
And the people who call generics inferior dont know what its like to choose
Shubham Mathur
December 13, 2025 AT 10:06India makes 40% of the world’s generics and we don’t have patent thickets or pay-for-delay because we believe in access over profit
My cousin in Mumbai gets the same metformin as you do in Ohio for 30 cents a pill
And guess what? It works the same
So why are we letting American corporations steal trillions from sick people? Because they can? Because they own politicians? Because we let them?
Stop pretending this is about science. It’s about power. And we’re losing.
Fix the system or get ready for more deaths disguised as ‘market dynamics’
Iris Carmen
December 15, 2025 AT 06:23my last script was $120 and now its $6 and i can actually afford to take it
also the generic looks like a rainbow gummy bear but hey it dont make me sick so 🤷♀️