Insulin Pump Therapy for Type 1 Diabetes: Pros, Cons, and How to Get Started
 Nov, 22 2025
Nov, 22 2025
For someone with type 1 diabetes, managing blood sugar isn’t just about checking numbers-it’s about living. And for many, insulin pump therapy offers a way to do that with more freedom, less guesswork, and fewer lows. But it’s not magic. It’s a tool. And like any tool, it works best when you understand how to use it-and when it fits your life.
What Is Insulin Pump Therapy?
Insulin pump therapy, also called continuous subcutaneous insulin infusion (CSII), delivers rapid-acting insulin through a small, wearable device. Instead of injecting insulin multiple times a day, the pump sends a steady trickle of insulin (called basal insulin) through a tiny tube or patch stuck under your skin. When you eat, you press a button to deliver a burst of insulin (a bolus) based on your carbs and blood sugar.
Modern pumps are tiny-about the size of a deck of cards-and weigh less than 4 ounces. Some, like the Omnipod 5, stick directly to your body with no tubes. Others, like the Medtronic MiniMed 780G or Tandem t:slim X2, use thin tubing that connects to a catheter. Most now connect to a continuous glucose monitor (CGM), so they can automatically adjust insulin based on your real-time glucose levels. This is called automated insulin delivery (AID) or a hybrid closed-loop system.
These aren’t new inventions. The first pump came out in 1978. But today’s models are smarter, smaller, and more reliable than ever. And they’re not just for adults-FDA-approved for kids as young as 2.
Pros of Insulin Pump Therapy
If you’ve ever struggled with unpredictable blood sugar swings, frequent low blood sugars at night, or the mental load of counting injections, a pump might help.
- Lower HbA1c: Studies show people using pumps have, on average, 0.37% lower A1c than those on multiple daily injections. That might sound small, but it means fewer long-term complications.
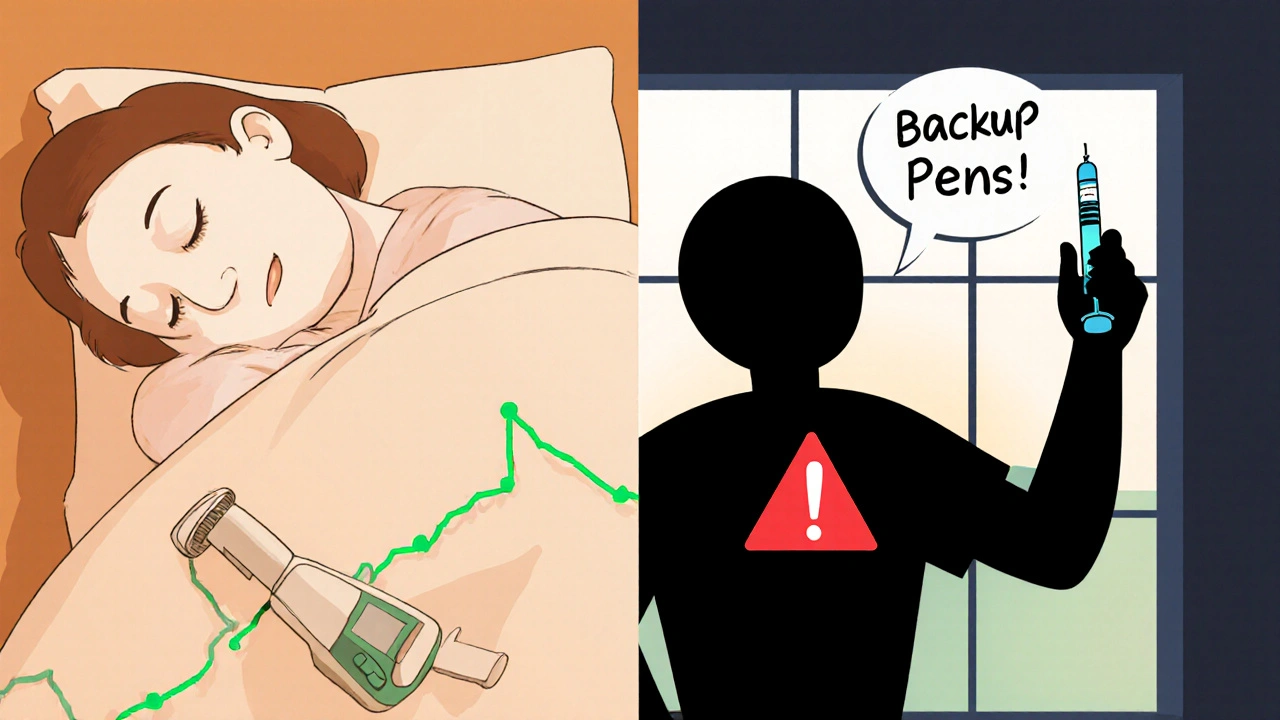
- Fewer nighttime lows: Pump users report a 32% drop in nocturnal hypoglycemia. Automated systems can predict a drop and slow or stop insulin before it happens.
- More flexibility: No more planning meals around injection times. Want to eat dinner at 9 p.m.? Go ahead. Need to skip a snack? The pump adjusts. You can change your basal rate for workouts, sleep, or stress with just a few taps.
- Less injection trauma: You only change the infusion set every 2-3 days. No more poking yourself 4-6 times a day.
- Better quality of life: In a survey of over 22,000 pump users, 82% said their quality of life improved. Many say they feel less anxious about diabetes and more in control.
One user on Reddit wrote: "The auto-basal adjustment has reduced my overnight lows from 3-4 a week to maybe once a month." That’s the kind of change that reshapes sleep, work, and relationships.
Cons of Insulin Pump Therapy
But it’s not all smooth sailing. Pumps come with real downsides that many people don’t talk about until they’re already wearing one.
- Technical failures: About 15% of users experience an insulin delivery interruption at least once a month. That could mean a clogged catheter, air in the line, or a pump malfunction. If insulin stops flowing for 4-6 hours, you can develop diabetic ketoacidosis (DKA)-a medical emergency.
- Constant monitoring: A pump isn’t "set and forget." You still need to check your blood sugar 4-6 times a day or rely on a CGM. You have to count carbs, enter boluses, and troubleshoot alarms. If you’re overwhelmed by tech, this can add stress, not reduce it.
- Skin issues: About 45% of users report irritation, redness, or infection at the infusion site. Some people just can’t tolerate the adhesive or the constant presence of a device on their skin.
- Alarm fatigue: Pumps beep for low battery, low insulin, blocked lines, high glucose, low glucose. Over time, the noise becomes background noise-and that’s dangerous. One user on TuDiabetes.org shared: "My pump failed during a family vacation. I didn’t notice until I felt sick. By then, I had DKA in 5 hours. Now I always carry backup pens."
- Cost and insurance: The pump itself costs $5,000-$7,000. Supplies (infusion sets, reservoirs, CGM sensors) run $3,000-$5,000 a year. While 90% of U.S. patients get insurance coverage, some still face $100-$500 copays after deductibles. And 22% report being denied coverage outright.
And then there’s the emotional side. Dr. Anne Peters warns that pumps aren’t ideal for people with eating disorders or high anxiety about technology. If you’re already overwhelmed by diabetes, adding another layer of complexity might backfire.
Who Is a Good Candidate for an Insulin Pump?
Not everyone needs or should get a pump. The Association of Diabetes Care & Education Specialists (ADCES) recommends considering one if you have:
- A1c above 7.5% despite optimized insulin injections
- Frequent or severe low blood sugars, especially at night
- Low blood sugar unawareness (you don’t feel your lows coming)
- High glucose variability-your numbers swing wildly even with consistent habits
- Desire for more flexibility in eating, sleeping, or exercising
Children and teens often do very well on pumps. In fact, 45% of U.S. kids with type 1 diabetes use them, compared to 34% of adults. The ability to adjust basal rates for growth spurts, sports, and school schedules makes pumps especially useful for families.
But if you have trouble with fine motor skills, can’t read small screens, forget to check glucose, or dislike tech, a pump might not be the right fit. Some people do better with injections-even if their A1c is higher.
How to Get Started With an Insulin Pump
Getting a pump isn’t like ordering a new phone. It’s a medical decision that requires planning, training, and support.
- Talk to your care team: Start with your endocrinologist or diabetes educator. They’ll review your history, current insulin use, and lifestyle. They’ll also check if your insurance covers pumps and which models are approved.
- Choose your pump: The three main brands are Medtronic, Tandem, and Insulet. Each has different features:
| Pump Model | Type | Insulin Capacity | CGM Integration | Waterproof? | Minimum Age |
|---|---|---|---|---|---|
| Medtronic MiniMed 780G | Tubed | 300 units | Yes (Guardian 4) | Yes (up to 12 ft for 30 min) | 2 years |
| Tandem t:slim X2 with Control-IQ | Tubed | 300 units | Yes (Dexcom G6/G7) | Yes (pump body only) | 2 years |
| Insulet Omnipod 5 | Tubeless | 200 units | Yes (Dexcom G6/G7) | Yes (up to 3 meters for 30 min) | 2 years |
- Get trained: Most people need 3-5 sessions with a certified diabetes educator. You’ll learn how to insert the catheter, program basal rates, calculate boluses, troubleshoot alarms, and respond to high or low glucose alerts.
- Practice before switching: Many clinics let you use a simulator or practice pump first. You’ll learn how to handle a low glucose event without insulin delivery, or how to change a site under stress.
- Prepare for the first 2 weeks: The first 14 days are the hardest. You’ll likely make mistakes with bolus amounts, misplace your pump, or get frustrated with alarms. That’s normal. Keep a log of highs and lows. Call your educator if you’re stuck.
- Have a backup plan: Always carry insulin pens and syringes. In case the pump fails, you need a way to deliver insulin fast. Keep extra infusion sets, batteries, and alcohol wipes in your bag.
Cleveland Clinic reports that 70% of new users need 2-3 weeks to feel confident. Don’t rush. It’s okay to take your time.
What’s Next for Insulin Pump Technology?
The future is getting even smarter. In 2023, the ADA updated its guidelines to recommend automated insulin delivery systems as the preferred option for all people with type 1 diabetes who can access them.
Upcoming pumps include:
- Medtronic MiniMed 880G with SmartGuard Extended (expected late 2024)-this extends insulin suspension during lows from 2 hours to 150 minutes.
- Beta Bionics iLet Bionic Pancreas (in phase 3 trials)-this device calculates insulin and glucagon needs automatically without carb counting.
By 2027, experts predict 65% of new pediatric type 1 diabetes diagnoses will start on a hybrid closed-loop system. That’s up from 32% in 2022.
But technology alone won’t fix everything. The biggest barrier now isn’t the pump-it’s access. Insurance denials, high out-of-pocket costs, and lack of provider training still keep many people from getting what could help them most.
Real Talk: Is It Worth It?
There’s no single right answer. One person’s freedom is another’s burden.
If you’re tired of injecting, sick of nighttime lows, and ready to take on a little more tech in exchange for more control-then yes, a pump can change your life.
If you’re already overwhelmed, afraid of tech, or unsure you’ll stick with monitoring and troubleshooting-then injections might still be your best bet. And that’s okay.
The goal isn’t to use the newest gadget. The goal is to live well with type 1 diabetes. For some, that means a pump. For others, it means pens. For both, it means support, education, and patience.
Can children use insulin pumps?
Yes. Modern insulin pumps are FDA-approved for children as young as 2 years old. Many pediatric endocrinologists recommend starting pumps early because they offer better glucose control during growth spurts, school activities, and unpredictable eating habits. Pumps also reduce the burden on caregivers by allowing remote bolus delivery and automated adjustments.
Do I still need to check my blood sugar if I use a pump?
Yes. Even with a CGM, you should still verify your glucose with a fingerstick at least once a day, especially if your CGM readings seem off, you’re feeling symptoms of high or low blood sugar, or you’re making a big insulin adjustment. Pumps rely on accurate data-if your sensor is wrong, the pump will make the wrong decision.
What happens if my insulin pump breaks?
If your pump stops working, you must switch to insulin injections immediately. Never go without insulin for more than a few hours. Always carry backup insulin pens and syringes. Most pump manufacturers offer loaner devices while yours is repaired or replaced. Contact your provider right away if you experience a failure.
Are insulin pumps covered by insurance?
Most U.S. insurance plans, including Medicare and Medicaid, cover insulin pumps if you have type 1 diabetes and meet clinical criteria. However, coverage varies. Some require proof of A1c above 7.5%, failed injection therapy, or frequent hypoglycemia. You may still pay $100-$500 in copays after meeting your deductible. If denied, ask for a letter of medical necessity from your doctor.
Can I swim or shower with an insulin pump?
Yes-but it depends on the model. The Omnipod 5 and Medtronic MiniMed 780G are waterproof up to 3 meters for 30 minutes, so you can swim or shower with them on. Tubed pumps are not fully waterproof; you’ll need to disconnect and cover the site with a waterproof dressing. Always check your pump’s manual for specific water resistance ratings.
How long do insulin pumps last?
Most insulin pumps are designed to last 4-5 years before needing replacement. Insurance typically covers a new pump every 4-5 years if you still meet clinical criteria. Some users upgrade sooner for newer features, but it’s not required. Always keep your current pump’s supplies stocked until you receive your replacement.
If you’re considering a pump, start with your care team-not a YouTube review or a Reddit thread. Talk to someone who’s been using one for years. Try a simulator. Ask about backup plans. And remember: your diabetes management should fit your life, not the other way around.
Lisa Lee
November 23, 2025 AT 20:07Ugh, another tech bro pushing pumps like they’re the holy grail. I’ve had mine for three years and it’s cost me more in copays than my car payment. And don’t even get me started on the alarms at 3 a.m. - my dog barks louder than this thing. If you’re gonna live like a cyborg, at least make it worth it.
Kezia Katherine Lewis
November 24, 2025 AT 09:09From a clinical perspective, the shift toward hybrid closed-loop systems represents a paradigmatic evolution in exogenous insulin delivery kinetics. The reduction in glycemic variability, particularly in nocturnal hypoglycemic events, correlates strongly with improved neurocognitive outcomes in pediatric cohorts. However, the adherence burden remains non-trivial - especially when considering the psychosocial load of continuous sensor dependency and algorithmic autonomy.
Dalton Adams
November 26, 2025 AT 03:39First off - anyone who says "pumps are just for tech nerds" clearly hasn’t read the ADA 2023 guidelines. 😏 Second - the Medtronic 780G isn’t even the best option anymore. Tandem’s Control-IQ with Dexcom G7 has 98% accuracy in predictive suspension, and the Omnipod 5’s AI is literally learning your patterns. And no, you don’t "need" to check fingersticks daily - if your CGM is calibrated properly, you’re wasting time. Also, your insulin capacity isn’t 300 units - it’s 200 for Omnipod. You’re wrong. Again.
Laurie Sala
November 27, 2025 AT 05:46I tried the pump... I really did... I cried every night for two weeks... I had a panic attack when it beeped during my daughter’s recital... I felt like I was being punished for wanting to eat pizza without calculating carbs... I hated the sticky patch... I hated the beeping... I hated the way my arm looked... I felt like a robot... I felt like a failure... I went back to pens... and for the first time in years... I slept... I actually slept...
Matthew Mahar
November 28, 2025 AT 01:32Man, I read this whole thing and honestly? I’m so glad I found this. I’ve been on pens for 8 years and was scared to even look at a pump. But now I’m thinking maybe… just maybe… I could give it a shot. I’ve had 3 DKA episodes in the last year. I’m tired of being scared to sleep. I don’t know how to start, but I’m gonna call my doc tomorrow. Thanks for not making me feel dumb for not knowing this stuff sooner.
Bryson Carroll
November 29, 2025 AT 01:48Everyone’s so obsessed with the tech but no one talks about the real cost - emotional and financial. You think you’re getting freedom but you’re just trading injection trauma for algorithmic anxiety. And let’s be real - 22% denied coverage? That’s not a glitch. That’s systemic. The system wants you to be sick enough to need a pump but not rich enough to afford it. This isn’t medicine. It’s a luxury product wrapped in a medical narrative.
Olanrewaju Jeph
November 30, 2025 AT 03:59As someone from Nigeria where insulin is a daily struggle just to get, I see this as a miracle - but also a reminder of how unequal healthcare is. In Lagos, people reuse syringes because they can’t afford new ones. Here, we argue over which pump has better waterproofing. I’m grateful for the tech, but let’s not forget the global reality. Maybe the real innovation isn’t the pump - it’s making it accessible to everyone.
Karla Morales
November 30, 2025 AT 06:37Let’s be real - if you’re not using a CGM with your pump, you’re doing it wrong. 🤦♀️ And if you think you can skip training? You’re one missed bolus away from DKA. I’ve seen it. I’ve lost friends to it. This isn’t a gadget. It’s a life-support system. And yes - you need backup pens. Always. No exceptions.
Javier Rain
December 1, 2025 AT 21:04Just got my Omnipod 5 last month - and wow. I went from 10+ lows a week to 1 in a month. I slept through the night. I ate tacos at midnight. I didn’t panic when my glucose spiked after a workout. It’s not perfect - I still hate changing the site - but it gave me my life back. If you’re on the fence? Do the training. Get the backup pens. Try the simulator. You’ve got nothing to lose but the fear.
Demi-Louise Brown
December 2, 2025 AT 05:19Insulin pumps are tools. Not solutions. Not miracles. Not punishments. They fit some lives. They don’t fit others. And that’s okay. Your diabetes management should serve you - not the other way around. If pens work for you, keep using them. If pumps help you breathe again, go for it. No judgment. Just care.
Pramod Kumar
December 2, 2025 AT 12:27Bro, I remember when my cousin in Mumbai used a syringe she borrowed from her neighbor’s kid because she couldn’t afford insulin. Now here we are, arguing over whether the pump is waterproof to 3 meters. I’m not mad - I’m just… overwhelmed. The tech is beautiful. But the gap between who gets it and who doesn’t? That’s the real emergency. Maybe the next innovation isn’t in the pump - it’s in the policy.
Suresh Ramaiyan
December 2, 2025 AT 15:14It’s funny - we talk about pumps like they’re the answer to diabetes. But diabetes isn’t a problem to be solved. It’s a condition to be lived with. Some people find peace in needles. Others find it in algorithms. Neither is better. Both are valid. The real question isn’t which device you use - it’s whether you feel seen, supported, and safe while using it.
Katy Bell
December 4, 2025 AT 04:46My 8-year-old got her Omnipod last year. She calls it her "magic bracelet." She doesn’t care about basal rates or CGMs. She just knows it helps her play soccer without passing out. And honestly? That’s all that matters. The tech is cool. But the kid? She’s the real hero.