Mineral Bone Disorder in CKD: Understanding Calcium, PTH, and Vitamin D
 Jan, 16 2026
Jan, 16 2026
What Is CKD-Mineral and Bone Disorder?
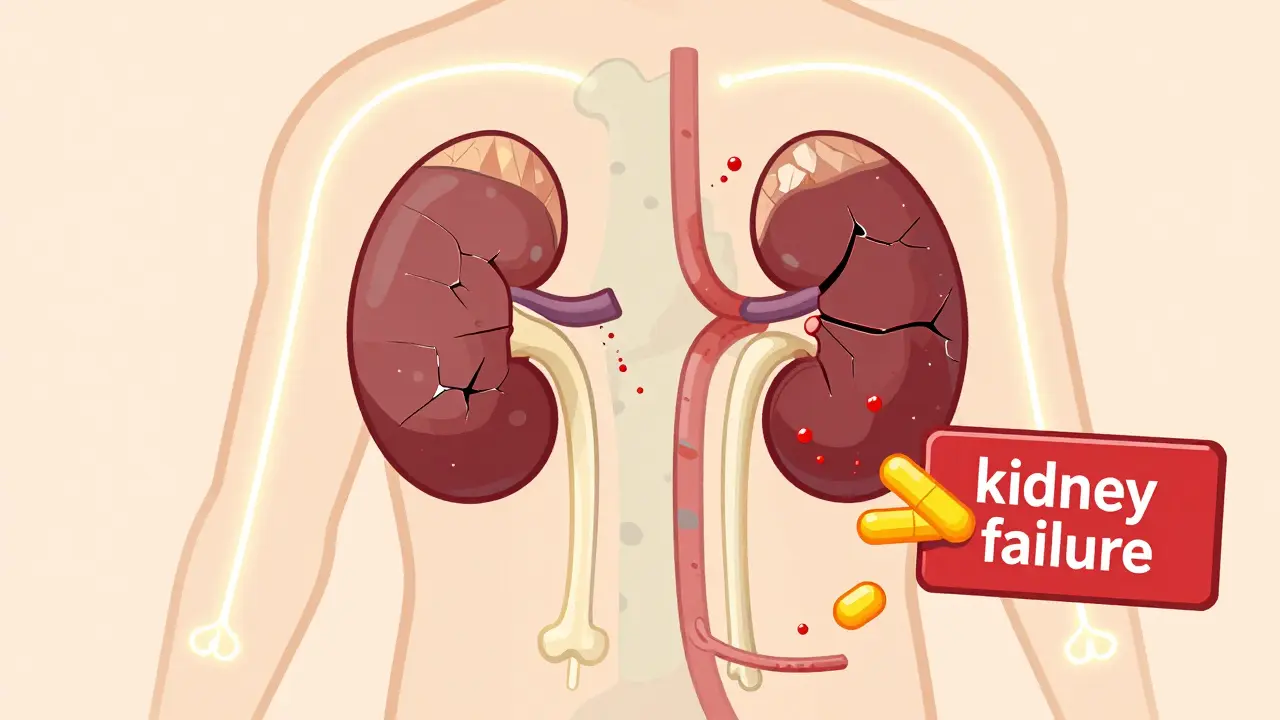
When your kidneys start to fail, they don’t just stop filtering waste-they also lose their ability to keep your bones and blood chemistry in balance. This is called CKD-Mineral and Bone Disorder (CKD-MBD). It’s not just a bone problem. It’s a full-body mess involving calcium, phosphate, parathyroid hormone (PTH), and vitamin D. And it affects nearly everyone with moderate to severe kidney disease.
Before 2006, doctors called this condition ‘renal osteodystrophy’-focusing only on bone damage. But research showed the damage goes deeper. Blood vessels calcify. The heart gets strained. Bones become brittle even if they look dense on a scan. That’s why experts now treat CKD-MBD as one system-wide problem, not three separate ones.
The Three-Part Cycle: Phosphate, PTH, and Vitamin D
Here’s how it all connects:
- Your kidneys can’t flush out phosphate anymore as kidney function drops below 60 mL/min. So phosphate builds up.
- High phosphate triggers your body to make more FGF23, a hormone that shuts down vitamin D activation.
- Without enough active vitamin D, your gut can’t absorb calcium. Your blood calcium drops.
- Your parathyroid glands, sensing low calcium, go into overdrive and pump out too much PTH.
- High PTH pulls calcium out of your bones to raise blood levels-making them weak.
- At the same time, phosphate and calcium combine in your blood vessels, turning them stiff and brittle.
This loop keeps spinning. The worse your kidneys get, the harder your body fights back-and the more damage it does.
Why Calcium Isn’t Always the Answer
Many people assume low calcium means you need more calcium pills. But in CKD, that’s often the wrong move.
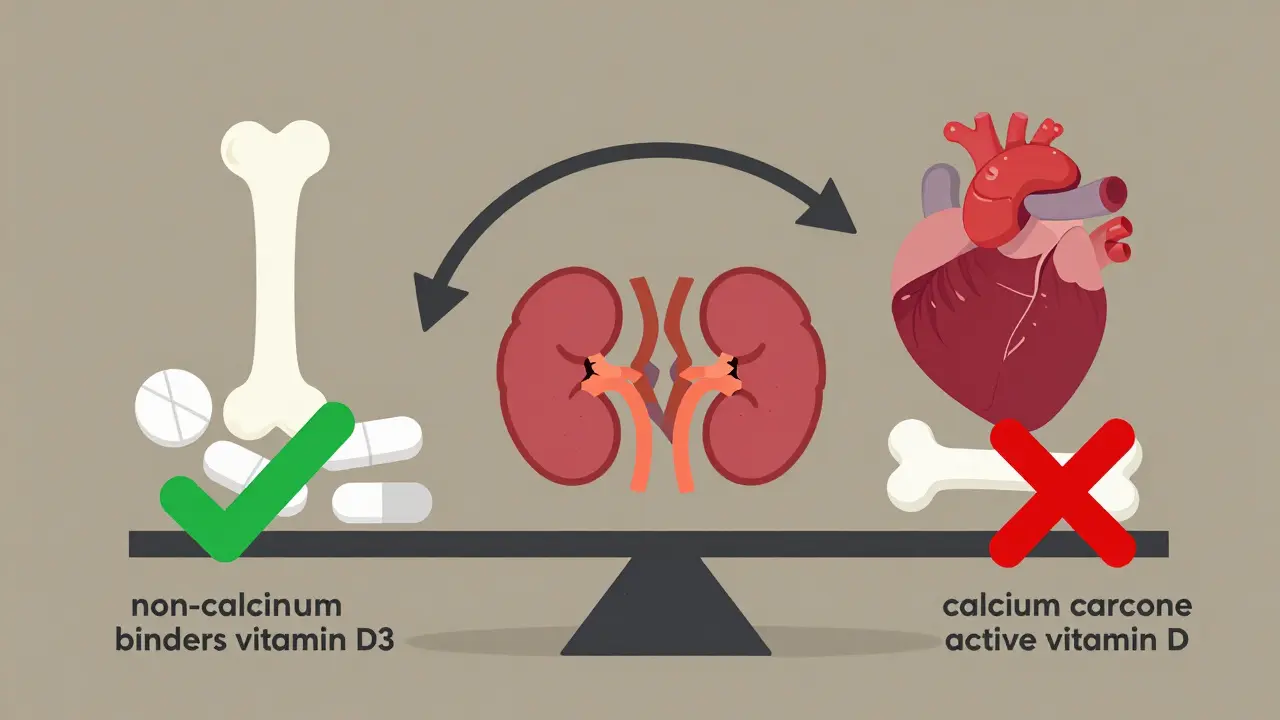
Doctors aim to keep serum calcium between 8.4 and 10.2 mg/dL. Too low? You risk bone loss. Too high? You risk calcium deposits in your heart and arteries. And here’s the catch: calcium-based phosphate binders (like calcium carbonate) can push levels too high. That’s why guidelines now limit calcium intake from binders to no more than 1,500 mg per day.
Instead of loading up on calcium, many patients are switched to non-calcium binders like sevelamer or lanthanum. These trap phosphate in the gut without adding calcium to the blood. They’re pricier, but they don’t speed up vascular calcification.
PTH: Too High or Too Low? Both Are Dangerous
Parathyroid hormone (PTH) is supposed to help regulate calcium. But in CKD, it becomes a runaway train.
Normal PTH? Around 10-65 pg/mL. In Stage 3 CKD, 40% of patients already have PTH above 65. By Stage 5 (dialysis), over 80% are above 300. That’s not just high-it’s toxic.
But here’s the twist: if PTH drops too low-below 150 pg/mL-you get something called adynamic bone disease. Your bones stop remodeling. They become dense but brittle. Fractures happen anyway, even if bone scans look normal.
That’s why doctors don’t just chase lower PTH. They aim for a target range: 2 to 9 times the upper limit of normal for your lab’s assay. For many, that’s 150-600 pg/mL. Too high? Use a calcimimetic like cinacalcet or etelcalcetide. Too low? Maybe you need less phosphate binder or even a break from vitamin D therapy.
Vitamin D: The Missing Link
Most people with CKD are vitamin D deficient. Studies show 80-90% of Stage 3-5 patients have levels below 20 ng/mL. But not all vitamin D is the same.
There’s 25-hydroxyvitamin D (the storage form) and 1,25-dihydroxyvitamin D (the active form). Your kidneys can’t make the active form anymore. So giving you calcitriol (the active version) used to be standard.
Now? Experts say: start with nutritional vitamin D-cholecalciferol (D3). Give 1,000-4,000 IU daily to raise 25(OH)D above 30 ng/mL. It’s safer, cheaper, and linked to a 15% lower risk of death.
Active vitamin D (calcitriol, paricalcitol) is only used if PTH is sky-high-over 500 pg/mL-and even then, only if phosphate is under control. Why? Because active vitamin D boosts calcium and phosphate absorption. If you’re already high on both, you’re feeding the calcification fire.
What Happens to Your Bones and Blood Vessels?
Two silent killers: broken bones and clogged arteries.
People on dialysis are 4-5 times more likely to break a hip than someone their age without kidney disease. And here’s the surprise: up to 60% of dialysis patients have low bone turnover. Their bones aren’t crumbling from too much PTH-they’re freezing up. No new bone forms. No old bone gets repaired. They’re like concrete that never sets.
At the same time, 75-90% of dialysis patients have vascular calcification. By age 50, their arteries look like those of a 70-year-old with heart disease. Coronary artery calcification scores are 3-5 times higher. That’s why half of all deaths in CKD are from heart attacks or strokes-not kidney failure.
It’s not coincidence. The same minerals that weaken your bones also harden your arteries. That’s why you can’t treat one without the other.
How Is It Diagnosed?
You won’t feel CKD-MBD until it’s advanced. That’s why labs are your best friend.
Every 3-6 months, you should have:
- Serum calcium
- Serum phosphate
- Intact PTH
- 25-hydroxyvitamin D
- Bone-specific alkaline phosphatase (BSAP) or PINP (if available)
These aren’t just numbers. They tell a story. High phosphate + high PTH + low vitamin D? Classic CKD-MBD. Low PTH + normal calcium? Watch out for adynamic bone disease.
Bone biopsy is the gold standard-but it’s invasive. Only 5% of patients get one. Most rely on the lab markers and clinical picture. If your PTH is dropping fast and your BSAP is low, your bone is likely slowing down.
For vascular calcification, a simple chest X-ray can show calcium in arteries. But CT scans (Agatston score) are more accurate. If you’re on dialysis, ask for one every 1-2 years.
What’s New in Treatment?
CKD-MBD treatment is changing fast.
Five years ago, cinacalcet was the go-to for high PTH. Now, etelcalcetide-a weekly injection-cuts PTH even more, with fewer side effects. It’s becoming the first-line choice for many.
And then there’s romosozumab. Originally for osteoporosis, it’s now being tested in CKD. It blocks sclerostin, a protein that shuts down bone formation. In early trials, it boosted bone density by 30-40% in Stage 3-4 CKD patients. No more frozen bones.
Even more exciting? Research on Klotho. This protein, made by the kidneys, helps FGF23 do its job. When kidneys fail, Klotho drops. Animal studies show giving Klotho reduces artery calcification by half. Human trials are coming.
The big shift? Start early. FGF23 rises years before phosphate does. By Stage 3 CKD, your body is already struggling. Testing vitamin D and phosphate every 6-12 months from Stage 3 onward could change outcomes.
What You Can Do
You can’t fix your kidneys overnight. But you can take control of the minerals.
- Watch your phosphate. Avoid processed foods, colas, and packaged snacks-they’re loaded with hidden phosphate additives.
- Get your vitamin D checked. If it’s low, ask for D3, not the active form.
- Take phosphate binders with meals. If you forget, phosphate gets absorbed.
- Ask about your PTH trend-not just one number. Is it rising? Falling? Stable?
- Don’t self-prescribe calcium. Talk to your nephrologist first.
It’s not about perfection. It’s about balance. One small change-like swapping soda for water-can lower phosphate by 15%. One regular vitamin D test can prevent years of bone loss.
Final Thought: It’s a System, Not a Symptom
CKD-MBD isn’t something you treat with one pill. It’s not a bone problem. It’s not a calcium problem. It’s not even just a kidney problem.
It’s the body’s entire mineral system breaking down-and your kidneys are the first to fail. But that doesn’t mean you’re powerless. With the right labs, the right meds, and the right diet, you can slow it down. You can protect your bones. You can protect your heart.
The goal isn’t to cure it. It’s to outsmart it.
Is CKD-MBD the same as osteoporosis?
No. Osteoporosis is bone loss due to aging or hormonal changes, usually with normal mineral levels. CKD-MBD involves abnormal calcium, phosphate, and PTH levels caused by kidney failure. The bone damage looks different under a microscope, and the treatment is completely different. You can have both at the same time, but they need separate management.
Can vitamin D supplements fix CKD-MBD?
Not alone. Nutritional vitamin D (D3) helps correct deficiency and lowers death risk, but it won’t fix high phosphate or high PTH. In fact, giving active vitamin D (calcitriol) without controlling phosphate can make vascular calcification worse. Vitamin D is one piece of a larger puzzle.
Why do I need phosphate binders if I’m not eating much?
It’s not about how much you eat-it’s about what you eat. Processed foods, fast food, and even some medications contain phosphate additives that are 90% absorbed. You don’t need to eat a lot to get too much phosphate. Binders trap it in your gut before it enters your blood, regardless of portion size.
What happens if I miss my phosphate binders?
Each missed dose means more phosphate gets absorbed. Over weeks, that adds up. A single meal without binders can spike your phosphate by 0.5-1.0 mg/dL. That may seem small, but over time, it increases your risk of heart problems and bone fractures. Take them with every meal and snack that contains protein.
Can CKD-MBD be reversed?
Not fully-but it can be stopped or slowed. If caught early, bone turnover can improve, and vascular calcification may stabilize. In some cases, after a kidney transplant, mineral levels normalize and bone quality improves over 1-2 years. But once bone is severely damaged or arteries are heavily calcified, the damage is permanent. Early, consistent management is the best defense.
Should I avoid dairy to lower phosphate?
Not necessarily. Dairy is a good source of calcium and protein. The phosphate in milk is naturally bound and less absorbed than the phosphate in processed foods. You can still have small portions of milk or cheese. Avoid processed cheeses, flavored yogurts, and dairy alternatives with added phosphate. Focus on whole, unprocessed foods instead.
Jodi Harding
January 18, 2026 AT 09:03Also, the part about vascular calcification being the real killer? Yeah. My dad died of a heart attack at 58. His kidneys were bad, but no one ever connected the dots.
Kristin Dailey
January 20, 2026 AT 03:11Pat Dean
January 21, 2026 AT 10:44Andrew Qu
January 22, 2026 AT 23:08And yes, you can still have cheese. Just not the neon orange kind.
kenneth pillet
January 23, 2026 AT 00:34Danny Gray
January 24, 2026 AT 10:42Tyler Myers
January 25, 2026 AT 00:51Zoe Brooks
January 26, 2026 AT 14:47