Pain and Sleep: How to Break the Insomnia-Pain Cycle for Good
 Dec, 6 2025
Dec, 6 2025
When you’re in chronic pain, falling asleep isn’t just hard-it feels impossible. And when you finally do drift off, you wake up hours later with your body screaming louder than before. This isn’t bad luck. It’s a cycle. Pain keeps you awake. Poor sleep makes your pain worse. And before you know it, you’re stuck in a loop that feels impossible to escape.
The Cycle No One Talks About
Most people think pain causes insomnia. That’s only half the story. The truth? Insomnia doesn’t just happen because of pain-it actually makes pain worse. Research shows that people with poor sleep have a 56% higher chance of developing chronic pain within five years-even if they had no pain before. That’s not coincidence. It’s biology.
When you don’t sleep enough, your brain’s natural painkillers shut down. Endogenous opioids, the body’s own morphine-like chemicals, drop by 30-40%. At the same time, your body pumps out more inflammatory signals like IL-6, which heighten pain. Studies using brain scans show sleep loss turns up the volume on your pain centers, like turning a thermostat too high. You start feeling pain from things that used to be harmless-a light touch, a chair that’s slightly too hard, even the weight of a blanket.
For someone with fibromyalgia, arthritis, or lower back pain, this means a single night of bad sleep can turn a manageable 4/10 ache into an 8/10 flare-up. And it doesn’t just last one day. One patient on Reddit described how four nights of broken sleep sent her fibromyalgia into a tailspin that took two weeks to recover from-even after her sleep improved.
What’s Really Happening in Your Body
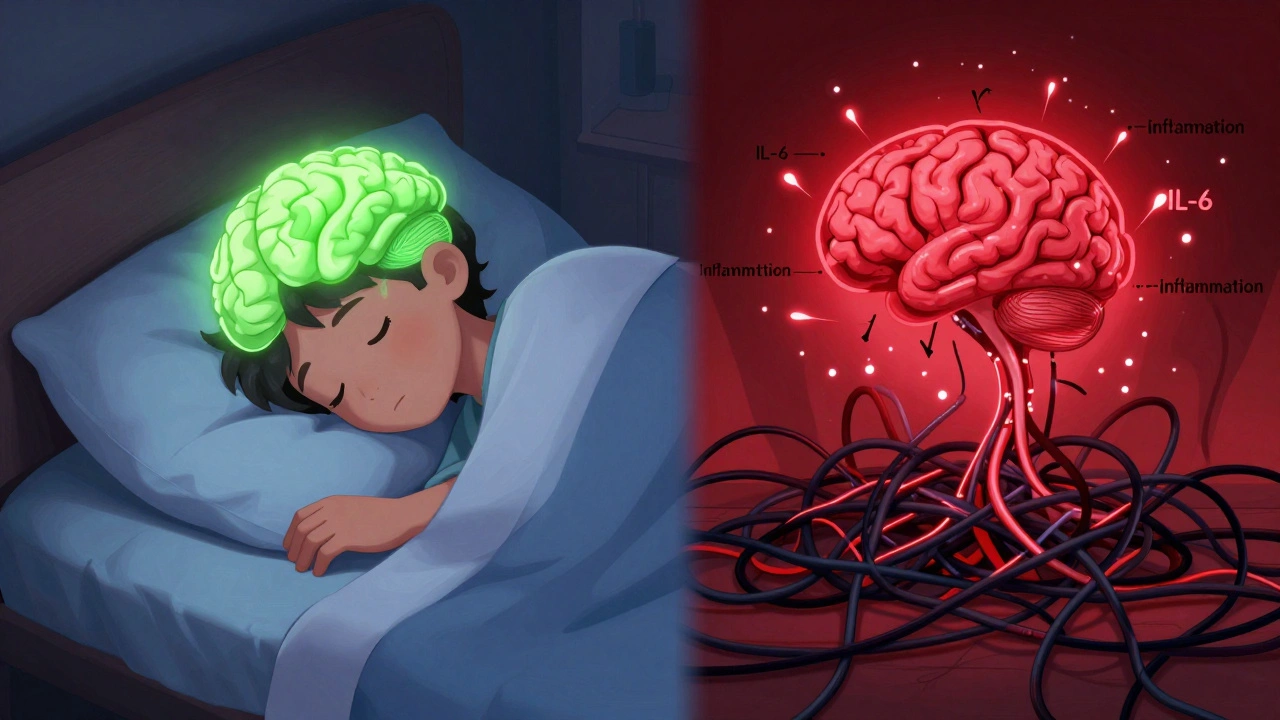
It’s not just about feeling tired. Your nervous system is rewiring itself. Sleep deprivation disrupts dopamine, a chemical that helps regulate both movement and pain relief. When dopamine drops by 20-30% after poor sleep, your body loses its ability to naturally dampen pain signals. At the same time, your brain’s pain control system becomes hypersensitive. You’re not imagining the pain. Your brain is literally interpreting normal sensations as dangerous.
Even your immune system gets involved. Lack of sleep increases pro-inflammatory cytokines by 25-35%. That means more swelling, more stiffness, more burning. For people with conditions like rheumatoid arthritis or chronic low back pain, this is a double hit: inflammation from the disease gets worse, and your body’s defenses can’t calm it down because sleep isn’t there to help.
And then there’s the kappa opioid receptor-a recently discovered player in this cycle. Researchers at the University of Arizona found that targeting this receptor improved sleep quality by 40-60% in animal models of chronic pain. Human trials are now underway, and early results show a 30-35% improvement in sleep and a 25-30% drop in pain scores. This isn’t science fiction. It’s the next frontier in treatment.
The Numbers Don’t Lie
Let’s look at what happens when pain and sleep collide:
- Chronic pain patients lose 45-60 minutes of sleep every night compared to healthy people.
- They take 25-30 minutes longer to fall asleep-and wake up 62 minutes per night on average (healthy people wake up 35 minutes).
- Only 40% of chronic pain patients report good sleep quality, compared to 85% of the general population.
- 54% of chronic pain patients meet the clinical diagnosis for insomnia-nearly five times higher than the general public.
- Those with both pain and insomnia report 35-45% higher pain intensity and 50% worse daily functioning.
These aren’t abstract stats. They’re the daily reality for over 1.5 billion people worldwide. And here’s the kicker: most doctors still treat pain and sleep as separate problems. But if you only fix one, the other pulls you right back down.
Why Over-the-Counter Sleep Aids Don’t Work
You’ve probably tried melatonin. Maybe diphenhydramine. Or those herbal gummies with valerian root. The Arthritis Foundation found that 72% of chronic pain patients have tried OTC sleep aids. But only 35% say they helped long-term. And 42% say they woke up groggy the next day-making their pain even worse.
Why? Because these pills don’t fix the root problem. They just mask symptoms. Melatonin might help you fall asleep faster, but if your brain is flooded with inflammatory signals and your dopamine is low, you’ll still wake up in pain. And if you rely on them every night, your body stops responding. You need more than a quick fix-you need a reset.
The Only Treatment That Actually Breaks the Cycle
There’s one therapy that’s been proven again and again to break the pain-sleep cycle: Cognitive Behavioral Therapy for Insomnia (CBT-I).
Unlike sleeping pills, CBT-I doesn’t rely on chemicals. It retrains your brain. A typical program lasts 8-10 weeks, with weekly 50-60 minute sessions. You learn how to:
- Stop associating your bed with pain and frustration
- Reset your internal clock with consistent sleep timing
- Reduce the anxiety that keeps your nervous system on high alert
- Use relaxation techniques that calm your body’s pain response
The results? 65-75% of chronic pain patients see major improvements in sleep. And here’s the game-changer: 30-40% report a real drop in pain intensity. That’s not just better sleep. That’s less pain.
One study showed CBT-I increased sleep efficiency by 12-15 percentage points and cut time spent awake after falling asleep by 35-40 minutes. That’s the difference between lying there for an hour staring at the ceiling and actually sleeping.
And it’s not just in-person. Digital CBT-I programs like Sleepio have 60-65% success rates in chronic pain patients. The catch? Only about half finish the full program. Why? Because it takes effort. But so does living in constant pain.

What a Real Treatment Plan Looks Like
Breaking this cycle isn’t about one magic trick. It’s about building a system:
- Track your sleep and pain for two weeks. Use a simple diary: note when you got into bed, how long it took to fall asleep, how many times you woke up, how long you were awake, and your pain level each morning (on a scale of 1-10).
- Get screened. If your Insomnia Severity Index score is above 15, you have clinically significant insomnia that needs targeted help.
- Find a CBT-I specialist. Look for a therapist trained in both sleep and chronic pain. Not all therapists are the same. Ask if they’ve worked with chronic pain patients before.
- Combine with pain management. If you’re on opioids or NSAIDs, talk to your doctor about how they affect sleep. Some pain meds keep you awake or cause restless legs. Alternatives like gabapentin or low-dose nortriptyline can help both pain and sleep.
- Build a sleep-friendly environment. Keep your bedroom cool, dark, and quiet. Avoid screens 90 minutes before bed. Use white noise if your body is too alert. And if you can’t sleep after 20 minutes, get up. Go sit in another room with dim light. Don’t lie there stressing.
Patients who get this kind of integrated care report satisfaction ratings of 4.7 out of 5. Those who only get pain meds? 3.2. The difference? One treats the whole person. The other treats a symptom.
What’s Coming Next
The science is moving fast. In 2023, the NIH poured $12.7 million into research specifically targeting the pain-sleep cycle. There are 47 active clinical trials. One of the most promising? Kappa opioid receptor modulators. These aren’t opioids in the traditional sense-they don’t cause addiction or respiratory depression. Early trials show they improve sleep and reduce pain without the side effects of current drugs.
Researchers at Harvard and Massachusetts General Hospital have also identified 12 gene variants that link sleep regulation and pain sensitivity. That means one day, doctors might be able to predict who responds best to CBT-I versus medication, based on their DNA.
The market for integrated pain-sleep treatments is expected to hit $5.7 billion by 2028. Why? Because people are finally demanding better. And the data proves it: treating sleep isn’t optional. It’s essential.
You Don’t Have to Live Like This
If you’ve been told your pain is just part of life, that’s not true. If you’ve been told to just take a pill and sleep better, that’s not enough. The cycle is real-but it’s not permanent.
You can break it. Not with luck. Not with a miracle. But with the right tools. CBT-I works. It’s not easy. But it’s easier than living in pain every day, every night, for years.
Start tonight. Write down your sleep and pain for two weeks. Then find a therapist who understands both. You’re not broken. Your body is stuck in a loop. And loops can be undone.
Can poor sleep cause chronic pain even if I didn’t have it before?
Yes. Research shows people with chronic sleep problems have a 56% higher risk of developing chronic pain within five years-even if they had no prior pain. Sleep loss lowers your pain threshold and triggers inflammation, making your nervous system more sensitive over time.
Why don’t sleeping pills help with pain-related insomnia?
Sleeping pills don’t fix the underlying cause-they just suppress symptoms. They don’t restore your brain’s natural pain control systems, reduce inflammation, or reset your sleep-wake cycle. Many also cause next-day grogginess, which can worsen pain perception and reduce mobility.
Is CBT-I effective for people with severe pain?
Yes. Studies show CBT-I works even for people with severe fibromyalgia, arthritis, and neuropathic pain. It doesn’t eliminate pain, but it reduces how much it affects your sleep-and in turn, how much your sleep worsens your pain. Patients report 30-40% pain reduction after completing CBT-I.
How long does it take to see results from CBT-I?
Most people start seeing improvements in sleep within 2-3 weeks. Pain reduction usually follows after 4-6 weeks. The full 8-10 week program gives the best long-term results. Consistency matters more than speed.
Can I do CBT-I online?
Yes. Digital platforms like Sleepio and SHUTi have been tested in chronic pain populations and show 60-65% effectiveness. Completion rates are lower than in-person programs, but they’re still far more effective than medication alone. Look for programs designed specifically for chronic pain.
What should I ask my doctor about my sleep and pain?
Ask: "Could my sleep problems be making my pain worse?" and "Can you refer me to a specialist who treats both chronic pain and insomnia?" Also ask if they use the Insomnia Severity Index (ISI) to screen patients. If they don’t, it’s a sign they’re not treating the full picture.
Jane Quitain
December 7, 2025 AT 22:25i just tried that sleepio thing for 3 weeks and honestly? my back pain dropped from an 8 to a 4. i didnt even think it would work but now i actually sleep through the night. no more meds, no more gummies, just my phone and some breathing exercises. life changing.
Kurt Russell
December 8, 2025 AT 12:22LET ME TELL YOU SOMETHING. CBT-I ISN’T JUST A THERAPY-IT’S A REBELLION. YOU’RE NOT JUST SLEEPING BETTER, YOU’RE TAKING BACK YOUR NERVOUS SYSTEM FROM THE PAIN. I DID THIS AFTER 12 YEARS OF FIBROMYALGIA. I WENT FROM CRYING IN BED EVERY NIGHT TO WALKING MY DOG AT 6AM WITHOUT A CRUTCH. THIS ISN’T HOPE. THIS IS SCIENCE. AND IT WORKS. DO IT. NOW.
Desmond Khoo
December 10, 2025 AT 06:56bro i was skeptical too but after 4 weeks of sleepio i’m actually sleeping 6+ hours straight 😭 i used to wake up at 2am screaming because my hips felt like they were on fire. now? i just roll over and go back to sleep. also i stopped taking gabapentin. my doc was shocked. thank you for posting this 🙏
Louis Llaine
December 11, 2025 AT 19:56oh great. another ‘just do CBT-I’ post. because clearly the answer to chronic pain is… doing homework? i’ve got a 90-hour workweek, two kids, and a spine that feels like it’s been run over by a truck. you think i’ve got time to log my sleep like it’s a fitness tracker? 🙄
Ted Rosenwasser
December 13, 2025 AT 15:06While the CBT-I data is statistically significant, the sample sizes in most studies remain underpowered for heterogeneous populations. The kappa opioid receptor modulation findings from Arizona are promising, but phase II trials have yet to control for placebo response in fibromyalgia cohorts. Also, the 56% increased risk metric conflates correlation with causality-did they adjust for cortisol dysregulation or HPA axis activity? The real issue is epigenetic priming from chronic stress, not sleep alone.
Ashley Farmer
December 14, 2025 AT 02:38i read this and just cried. not because i’m sad-but because i finally feel seen. i’ve been told for years that my pain is ‘all in my head’ or ‘just stress’. but this? this explains exactly what’s happening. thank you for writing this. if you’re reading this and you’re hurting-you’re not broken. you’re just stuck in a loop. and loops can be undone. i’m starting sleepio tomorrow.
Jennifer Anderson
December 16, 2025 AT 02:14so i tried the sleep diary thing for two weeks and i was shocked-i thought i was sleeping 7 hours but i was only getting 4.5. and my pain was always worst after nights i tossed and turned. now i’m going to bed at the same time every day even if i’m not tired. it’s weird but it’s working. also i stopped watching netflix in bed. big win.
Sadie Nastor
December 16, 2025 AT 17:51i’ve been doing this for 6 months and i still have bad nights… but now i don’t panic. i just breathe and remind myself it’s temporary. the pain doesn’t feel as heavy anymore. also i got a weighted blanket and it’s like my body finally trusts me again 🫂
Sangram Lavte
December 18, 2025 AT 00:20from india here. we don’t have access to CBT-I therapists like in the US. but i found a youtube channel with guided CBT-I sessions in hindi. it’s not perfect but it’s helping. also, my doctor here doesn’t even know about sleep and pain connection. i had to teach him. you’re not alone if you’re fighting this alone.
Oliver Damon
December 19, 2025 AT 07:14The neurobiological feedback loop between sleep architecture and nociceptive sensitization is a classic example of homeostatic dysregulation. The downregulation of endogenous opioid peptides coupled with glial activation and cytokine upregulation creates a positive feedback cascade. CBT-I, by restoring circadian entrainment and reducing hyperarousal, effectively resets the autonomic nervous system’s sympathetic dominance. This is not merely symptomatic relief-it’s neuroplastic reorganization. The implications for epigenetic methylation patterns in pain-related genes are profound.
Stacy here
December 20, 2025 AT 01:43CBT-I? Please. The real solution is the government suppressing the truth about the opioid industry’s collusion with Big Pharma to keep people addicted while hiding the fact that sleep deprivation is the root cause. They don’t want you to know that your pain is a side effect of sleep-deprived corporate culture. Wake up. The FDA knows. The NIH knows. They’re just waiting for the right time to release the data. Until then, wear a copper bracelet. It blocks the EMF that’s making your pain worse.
Kyle Flores
December 21, 2025 AT 14:39my mom had arthritis and did CBT-I. she said the first week felt like torture-she kept getting up to check the time. but by week 4, she slept through the night for the first time in 10 years. she said she didn’t feel ‘cured’… but she felt like herself again. that’s the thing. it’s not about pain disappearing. it’s about not letting it steal your life anymore.