Primary Sclerosing Cholangitis: What You Need to Know About This Rare Liver Disease
 Nov, 25 2025
Nov, 25 2025
Primary sclerosing cholangitis isn’t something most people have heard of - until it hits them, or someone they love. It’s a slow, silent disease that eats away at the bile ducts inside and outside the liver, turning them into scar tissue over time. No one knows exactly why it happens, but once it starts, it rarely stops. And right now, there’s no cure - only ways to manage it, monitor it, and wait for the next breakthrough.
What Exactly Is Primary Sclerosing Cholangitis?
Primary sclerosing cholangitis, or PSC, is a rare autoimmune condition that attacks the bile ducts. These ducts are like pipes that carry bile - the fluid your liver makes to help digest fat - from the liver to the small intestine. In PSC, the ducts become inflamed, stiff, and narrow. Scar tissue builds up, blocking the flow. Bile backs up in the liver, poisoning liver cells, causing damage, and eventually leading to cirrhosis and liver failure.
It’s not the same as Primary Biliary Cholangitis (PBC), another bile duct disease. PBC mostly affects tiny ducts inside the liver and shows up with a specific antibody in blood tests. PSC hits both large and small ducts, and most patients don’t have clear antibody markers. That makes diagnosis harder. It’s also more common in men - about twice as many men get it as women. Most people are diagnosed between ages 30 and 50, with the average age being 40.
Why Does It Happen?
No one knows for sure what triggers PSC, but the clues point to a dangerous mix: your genes, your gut, and your immune system going rogue.
Over 20 gene variants have been linked to PSC, with the strongest tied to HLA-B*08:01 - a gene that helps your immune system recognize threats. But having the gene doesn’t mean you’ll get the disease. Something else has to set it off. That’s where the gut comes in.
Eight out of ten people with PSC also have inflammatory bowel disease, mostly ulcerative colitis. The connection is so strong that doctors now check for PSC in anyone newly diagnosed with colitis, and vice versa. Researchers believe bacteria in the gut leak through a damaged intestinal lining, travel to the liver via the bloodstream, and trigger an immune attack on the bile ducts. It’s like your body mistakes your own ducts for invaders.
Dr. Konstantinos Lazaridis from Mayo Clinic calls it a "perfect storm" - genetics, gut bacteria, and immune chaos all lining up at once. And while we don’t yet know what specific bacteria are to blame, we do know the gut-liver axis is central to the disease.
How Is It Diagnosed?
PSC is often found by accident. Many people have no symptoms at first. Blood tests might show elevated liver enzymes - especially alkaline phosphatase (ALP) - and that’s the first red flag. But elevated enzymes can mean many things. To confirm PSC, doctors need to see the damaged bile ducts.
The go-to test is MRCP - magnetic resonance cholangiopancreatography. It’s a non-invasive MRI scan that creates detailed pictures of the bile ducts. In PSC, they look like a string of beads, with narrow sections and wider ones. Sometimes, if the diagnosis is still unclear, doctors use ERCP - a more invasive procedure that involves threading a scope into the gut to inject dye and take X-rays. But ERCP carries risks, so it’s used only when needed.
There’s no single blood test for PSC. About half of patients test positive for p-ANCA, but that’s not specific enough to rely on. Biopsies of the liver can show scarring patterns, but they don’t always capture the full picture because the damage is patchy.

What Are the Symptoms?
Early on, many people feel fine. That’s why diagnosis often takes years - an average of 2 to 5 years, according to patient surveys.
When symptoms do show up, they’re frustrating and often misunderstood:
- Fatigue - the most common complaint. Not just tiredness. A deep, bone-weary exhaustion that doesn’t go away with sleep.
- Itching (pruritus) - so bad it feels like it’s coming from inside your bones. Worse at night. Many patients say it’s the worst part of living with PSC.
- Abdominal pain - usually in the upper right side, dull or achy.
- Jaundice - yellowing of the skin and eyes - happens when bile backs up badly.
- Chills and fever - signs of cholangitis, a dangerous infection of the bile ducts.
One Reddit user described the itching like "fire under the skin," and another said they’d wake up at 3 a.m. scratching until they bled. These aren’t exaggerations - they’re real experiences from people living with this disease every day.
What Happens Over Time?
PSC is progressive. It doesn’t jump - it creeps. The scarring slowly worsens. Experts divide it into four stages:
- Stage 1: Inflammation around the portal areas of the liver.
- Stage 2: Fibrosis spreads from the portal areas.
- Stage 3: Bridges of scar tissue connect different parts of the liver.
- Stage 4: Cirrhosis - the liver is hardened, shrunken, and failing.
From the time symptoms start, it takes about 12 to 15 years on average for cirrhosis to develop. But that varies. Some people stay stable for decades. Others decline quickly.
And then there’s the cancer risk. People with PSC have a 1.5% chance each year of developing cholangiocarcinoma - bile duct cancer. That adds up to a 10-15% lifetime risk. That’s why regular imaging and blood tests (like CA 19-9) are critical. Early detection of cancer is rare, and survival rates drop to just 10-30% after diagnosis.
What Treatments Are Available?
Here’s the hard truth: there is no drug that stops or reverses PSC.
Ursodeoxycholic acid (UDCA), once widely prescribed, has been shown in multiple studies to do nothing for survival or disease progression. In fact, high doses (over 28 mg/kg/day) may even increase risk. The European Association for the Study of the Liver (EASL) and the American Association for the Study of Liver Diseases (AASLD) now both say: don’t use it routinely.
So what do you do?
- Manage symptoms: For itching, doctors try rifampicin, naltrexone, or colesevelam. About half of patients find relief with one of these.
- Replace vitamins: Since bile isn’t flowing properly, fat-soluble vitamins (A, D, E, K) aren’t absorbed. Regular blood tests and supplements are essential.
- Watch for infection: Cholangitis is a medical emergency. If you have fever, chills, and pain, go to the hospital immediately. Antibiotics are needed fast.
- Screen for cancer: Annual MRCP scans and CA 19-9 blood tests are standard. Colonoscopies every 1-2 years if you also have ulcerative colitis.
Specialized centers - places with dedicated PSC clinics - have better outcomes. Patients there report 85% better symptom control than those treated in general liver clinics. If you have PSC, find a center that sees at least 50 PSC patients a year. Ask your doctor where those are.
What’s on the Horizon?
Hope is building - slowly, but it’s there.
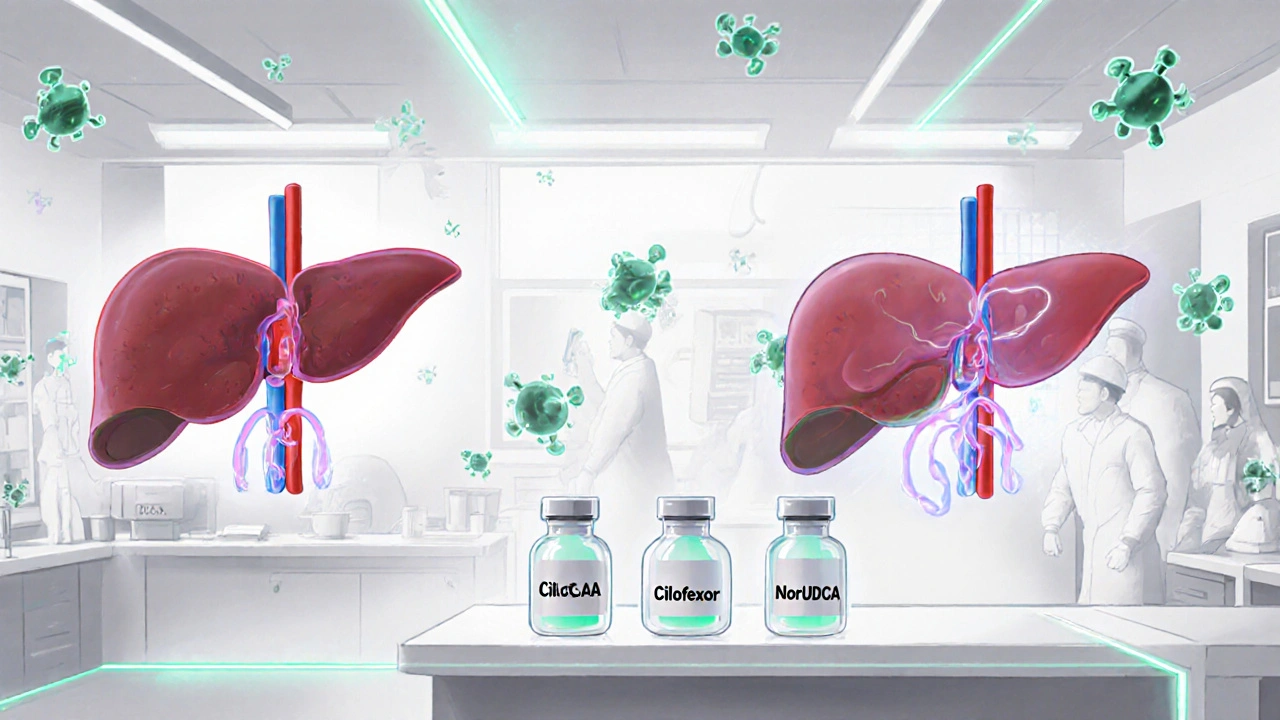
Several drugs are in late-stage trials:
- Obeticholic acid (OCA): A bile acid receptor agonist. In a 2023 trial, it lowered liver enzymes by 32% after 18 months. The FDA is reviewing it, but safety concerns remain.
- Cilofexor: A non-steroidal FXR agonist. It cut ALP levels by 41% in phase 2 trials. The EMA granted it orphan drug status in early 2023.
- NorUDCA: A modified version of UDCA. Early results show it may reduce bile duct damage without the risks of standard UDCA.
Dr. Andrew Manns from Hannover Medical School predicts we’ll have at least two approved disease-modifying drugs within five years. That’s not a cure, but it’s a chance to slow or even stop progression.
And then there’s liver transplant - the only proven life-saving treatment. For those with end-stage liver disease, transplant offers an 80%+ five-year survival rate. Many patients live decades after transplant. But it’s not a perfect fix: PSC can come back in the new liver, and transplant means a lifetime of immunosuppressants.
Living With PSC: What Patients Say
Patients aren’t just numbers. They’re people managing a disease that most doctors don’t fully understand.
On online forums, the most common complaints:
- "Doctors don’t take the fatigue seriously."
- "I’ve tried six different meds for itching. None worked well."
- "No one talks about the mental toll. You feel like you’re waiting to die."
But there’s also resilience. People are forming communities - like PSC Partners Seeking a Cure - with over 3,000 members worldwide. They share tips, clinical trial updates, and emotional support. One patient wrote: "I didn’t know I could live with this until I met others who were doing it."
And they’re pushing for change. Because research funding is tiny - just $8.2 million from the NIH in 2022, compared to $142 million for fatty liver disease. Patients are demanding more. And slowly, they’re getting it.
What Should You Do If You’re Diagnosed?
If you’ve just been told you have PSC, here’s what to do next:
- Find a specialist - not just any hepatologist. Look for a center with a PSC clinic or one that sees at least 50 PSC patients a year.
- Get baseline blood work: liver enzymes, vitamins A, D, E, K, and CA 19-9.
- Have an MRCP scan if you haven’t already.
- See a gastroenterologist for colon cancer screening if you have ulcerative colitis.
- Join a patient registry - like the PSC Partners registry - to help researchers.
- Learn to recognize signs of cholangitis: fever, chills, pain, jaundice. Act fast.
- Don’t take UDCA unless your doctor says it’s experimental and you’re in a trial.
PSC is not a death sentence. It’s a marathon. With good care, many people live full lives for decades. And the science is moving faster than ever.
Deirdre Wilson
November 26, 2025 AT 02:30So PSC is basically your liver’s plumbing getting clogged by your own immune system? Wild. I had no idea gut bacteria could trigger something like this. Feels like our bodies are just one leaky gut away from self-sabotage.
Bethany Buckley
November 27, 2025 AT 09:16It’s not merely a hepatic disorder-it’s a systemic epistemological rupture in the gut-liver axis, wherein microbial dysbiosis catalyzes an autoimmune misrecognition event mediated by HLA-B*08:01 polymorphisms. The body, in its tragicomic inefficiency, confuses bile duct epithelium for pathogen. 🤯
And yet, we persist in treating symptoms while ignoring the ontological root: the microbiome as silent architect of autoimmunity. The fact that UDCA is still prescribed is a testament to medical inertia, not efficacy. 🧪
Obeticholic acid? A step toward phenomenological intervention. But we must interrogate not just *how* it works-but *why* the immune system turned traitor in the first place. Is it the Western diet? Antibiotic overuse? The death of biodiversity in our guts? 🌱
And let’s not romanticize transplant. It’s not a cure-it’s a temporal reprieve wrapped in immunosuppressive chains. We’re trading one existential burden for another. The real revolution? Personalized microbiome reconstitution. That’s where the future lives.
Also, the itching? That’s not just pruritus. It’s the soul screaming through the skin. 🌑
Gina Banh
November 28, 2025 AT 07:17My cousin was diagnosed last year. They put her on rifampicin and it cut the itching by 70%. Not perfect, but life-changing. Also, she started taking vitamin D3 + K2 daily-her levels were abysmal. Don’t skip the vitamins. Seriously. And if you’re in the US, find a PSC center at Mayo, Johns Hopkins, or Cedars-Sinai. General hepatologists don’t get it.
Also, stop Googling ‘PSC prognosis’ at 2 a.m. You’ll spiral. The stats are scary, but progression is wildly individual. Some people are stable for 20+ years.
Ryan C
November 28, 2025 AT 22:48Actually, the p-ANCA positivity rate is closer to 60-70%, not 50%. And you’re wrong about UDCA-it’s not that it doesn’t work, it’s that high doses (>28 mg/kg) are harmful. Low-dose (13-15 mg/kg) still has some benefit in early-stage PSC, especially with cholestasis. EASL guidelines are overly cautious. Also, norUDCA isn’t just ‘modified UDCA’-it’s a choleretic that targets the small bile ducts directly. Phase 3 data looks promising. 📊
And yes, transplant survival is >80% at 5 years, but recurrence happens in 20-30% of cases. Most don’t mention that. 🤷♂️
Amanda Meyer
November 29, 2025 AT 11:24Thank you for writing this with such clarity. As someone whose partner was recently diagnosed, I’ve spent months drowning in medical jargon and half-truths. This is the first piece that made me feel like I actually understand what’s happening. The part about the gut-liver axis was eye-opening. We’re now researching clinical trials and connecting with PSC Partners. You’ve given us direction when we felt lost.
Dan Rua
December 1, 2025 AT 11:12Just wanted to say I’m so glad this post exists. I’ve been living with PSC for 8 years and still feel invisible in the medical world. The fatigue? Real. The itching? Nightmarish. But reading this and seeing others talk about it? It helps. I’m in a support group now. We meet every other week. If you’re out there and alone-reach out. You’re not crazy. You’re not alone. 🤝
Mqondisi Gumede
December 1, 2025 AT 22:23So this is why white people get sick all the time? Too clean. Too much vitamin D. Too much science. In Africa we don’t have this disease because we don’t live in sterile boxes. Our immune systems know what to fight. You overthink your body. Let it be. 🌍
Also why is everyone talking about transplants? Back home we just drink herbal tea and pray. Works better than all your drugs. You think your MRI is medicine? Nah. That’s just expensive photography.
Damon Stangherlin
December 2, 2025 AT 12:19Hey, just wanted to say I’ve been reading up on PSC since my brother got diagnosed. I’m not a doctor, but I’ve been helping him track his labs and remind him to take his vitamins. This post? Huge help. One thing I learned: if you’re ever in the ER with fever and pain, don’t wait. Cholangitis can kill fast. He almost missed it last year. Don’t be like us. Speak up. Advocate. You’re your own best advocate. 💪