Venlafaxine and Blood Pressure: What You Need to Know About Hypertension Risk
 Jan, 27 2026
Jan, 27 2026
Venlafaxine Blood Pressure Risk Calculator
Blood Pressure Risk Assessment
This tool estimates your risk of hypertension based on venlafaxine dosage, current blood pressure, and health factors. Always consult your doctor before making medication changes.
Your Risk Assessment
When you start taking venlafaxine for depression or anxiety, your doctor focuses on your mood. But there’s another number you need to watch-your blood pressure. Venlafaxine, sold under brands like Effexor and Effexor XR, is a powerful antidepressant that works on two brain chemicals: serotonin and norepinephrine. That dual action helps many people feel better, but it also comes with a quiet risk: rising blood pressure. This isn’t rare. It’s documented, predictable, and often overlooked.
How Venlafaxine Raises Blood Pressure
Venlafaxine doesn’t just lift your mood-it tightens your blood vessels. That’s because it blocks the reabsorption of norepinephrine, a chemical that acts like a natural stimulant. More norepinephrine in your system means your heart pumps harder and your arteries constrict. That’s how blood pressure climbs.
The effect isn’t the same for everyone. At low doses-under 150 mg per day-the impact is usually small. Most people see a rise of just 1 to 3 mmHg in diastolic pressure. But when the dose goes above 150 mg, especially beyond 300 mg, the risk jumps. Studies show that at these higher levels, about 13% of users develop clinically significant hypertension, compared to just 5% on placebo. That’s not a fluke. It’s a direct result of how the drug works.
Even more concerning? Some people see dangerous spikes at low doses. One case report described a 23-year-old man with no prior health issues whose blood pressure soared to 210/170 mmHg after only 10 months on 150 mg daily. He had no warning signs. No family history of high blood pressure. Just venlafaxine and a sudden, life-threatening spike. That’s why you can’t assume you’re safe just because you’re on a low dose.
Comparing Venlafaxine to Other Antidepressants
If you’ve tried an SSRI like sertraline or fluoxetine and it didn’t help, venlafaxine is often the next step. It’s more effective for treatment-resistant depression. But here’s the trade-off: SSRIs rarely affect blood pressure. Venlafaxine does-consistently and measurably.
Compared to older tricyclic antidepressants (TCAs), venlafaxine doesn’t cause dizziness from low blood pressure when standing up. That’s good. But it doesn’t let your pressure drop either. Instead, it pushes it up. Duloxetine, another SNRI, has a milder effect. Venlafaxine is the strongest blood pressure elevator in its class.
Even its metabolite, desvenlafaxine, raises blood pressure. Studies show a 0.66 to 3.41 mmHg increase in diastolic pressure at standard doses. That’s not huge-but it’s enough to matter if you’re already borderline hypertensive.
Who’s Most at Risk?
It’s not just about the dose. Some people are more vulnerable. If you already have high blood pressure, venlafaxine won’t necessarily make it worse-but it won’t help either. You’ll need tighter monitoring.
People with existing heart disease, kidney problems, or a history of stroke should be especially cautious. Even if your blood pressure is normal now, venlafaxine can push it into the danger zone. That’s why doctors are told to check your pressure before you start.
And it’s not just older adults. Younger people, even those in their 20s, can develop severe hypertension on venlafaxine. The case of the 23-year-old isn’t an outlier-it’s a warning.

What the Data Says: Real Numbers, Real Risks
Let’s look at hard numbers from real studies:
- At doses under 300 mg/day: average diastolic BP increase of 1-3 mmHg
- At doses over 300 mg/day: 13.1% of users develop clinically high BP (vs. 5% on placebo)
- Chronic use: up to 15 mmHg sustained diastolic rise over time
- Severe hypertension (diastolic >120 mmHg): occurs in less than 1% of users, but can be life-threatening
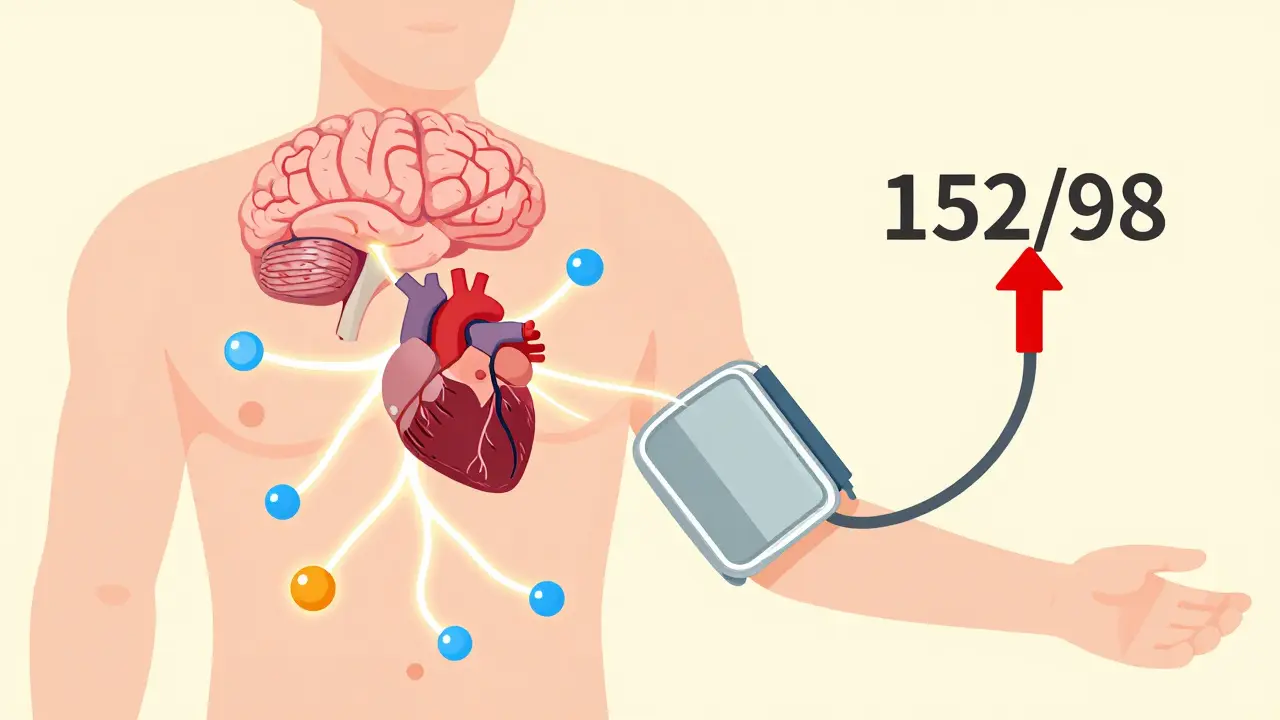
On patient forums, 68% of users reported measurable BP increases. About 12% hit readings above 140/90 mmHg-enough to be diagnosed as hypertensive. One user went from 118/76 to 152/98 in just three weeks on 75 mg. Another saw their pressure jump to 155/102 after two months on 37.5 mg. When they stopped, their BP returned to normal in three weeks.
But not everyone has bad experiences. Some people with unstable blood pressure say venlafaxine actually helped them stabilize. That’s rare, but it happens. The key is knowing your baseline and tracking changes.
How to Monitor Your Blood Pressure on Venlafaxine
If you’re on venlafaxine, you need a plan-not just a one-time check. Here’s what works:
- Baseline measurement: Get your blood pressure checked before you start the medication.
- First two weeks: Check it at home or at the clinic. Many people see the first rise within days.
- Week four: Another check. This is when the full effect often shows up.
- Monthly for the first 3 months: Especially if you’re on more than 150 mg/day.
- Quarterly after that: Keep checking, even if things seem fine.
Home monitoring is ideal. Buy a validated upper-arm cuff from a pharmacy. Write down your readings. Bring them to your appointments. Don’t wait for your doctor to ask.

What to Do If Your Blood Pressure Rises
If your readings consistently hit 140/90 or higher:
- Don’t panic-but don’t ignore it.
- Call your prescriber. Don’t stop the drug on your own.
- They may lower your dose, switch you to a different antidepressant, or add a blood pressure medication.
- In most cases, BP returns to normal within 1 to 4 weeks after stopping venlafaxine.
But if your systolic pressure hits 180 or higher, or your diastolic hits 110 or higher, that’s an emergency. Headache, blurred vision, chest pain, or nosebleeds along with high BP? Go to the ER. There’s a rare but real risk of posterior reversible encephalopathy syndrome (PRES)-a brain condition caused by sudden, severe hypertension. It’s treatable if caught early.
What the Experts Say
The American Psychiatric Association still lists venlafaxine as a first-line option for depression. But they also say: “Monitor blood pressure regularly.” The FDA’s label warns of “sustained blood pressure elevation.” The European Medicines Agency notes that while most cases are mild, severe hypertension can occur-even at low doses.
Dr. Arif Khan, who led the major 2005 study, says: “Concern about blood pressure shouldn’t stop you from using venlafaxine if it’s the right drug for you.” But he adds: “We need more data on patients with heart disease.”
Dr. Costas Kosmas, who reviewed the evidence in 2021, is clearer: “We’ve seen catastrophic outcomes from unmonitored venlafaxine use. This isn’t theoretical.”
Is Venlafaxine Right for You?
It’s not about avoiding venlafaxine. It’s about using it wisely.
If you’ve tried SSRIs and they didn’t work, venlafaxine could be the breakthrough you need. It’s one of the most effective antidepressants for treatment-resistant cases. But if you already have high blood pressure, heart disease, or a family history of stroke, you and your doctor need to weigh the risks carefully.
For many, the benefits outweigh the risks-especially with monitoring. For others, a different medication might be safer.
There’s no one-size-fits-all answer. But there is one rule: Never start venlafaxine without a baseline blood pressure check. Never stop checking after the first month.
Antidepressants change your brain. But they also change your body. Your blood pressure is one of the clearest signals that your body is responding. Pay attention to it. Track it. Talk about it. Your mind matters-but so does your heart.
Chris Urdilas
January 28, 2026 AT 12:11So let me get this straight - we’re giving people a drug that turns their blood pressure into a rollercoaster, but the only ‘warning’ is a footnote in a 40-page pamphlet? 🤡
My cousin took this for anxiety and ended up in the ER because his BP hit 200/130. He didn’t even know it was the meds until his cardiologist said, ‘Dude, you’re on venlafaxine, right?’
Yeah. That’s not a side effect. That’s a silent assassin with a prescription.
John Rose
January 28, 2026 AT 12:48This is an exceptionally well-researched and necessary piece. The data presented here is not only clinically significant but also under-discussed in primary care settings. Many patients are never informed of the cardiovascular implications of SNRIs, despite clear evidence of dose-dependent hypertension. Regular monitoring, as outlined, should be standard protocol - not an afterthought. Thank you for highlighting this critical gap in patient education.
Lexi Karuzis
January 30, 2026 AT 02:37Brittany Fiddes
January 31, 2026 AT 09:19Oh, how quaint - Americans are still being dosed with chemical cocktails while their doctors sip coffee and check off boxes. In the UK, we’ve had this conversation for decades. The NHS would never casually prescribe venlafaxine without a full cardiovascular screen - and even then, only as a last resort. Your healthcare system is a circus, and this is just the clown car with a stethoscope. 🇬🇧🫠
Colin Pierce
February 2, 2026 AT 02:26Biggest thing I learned after my own experience: check your BP before the first pill, then again at 7 days, 14 days, and 30 days. I went from 116/74 to 148/92 in 18 days on 75mg. Didn’t feel a thing. No headache, no dizziness - just a quiet, dangerous climb.
My doc didn’t even ask. I brought the readings in myself. We switched to bupropion. BP normalized in 2 weeks.
Don’t wait for symptoms. Track it. Document it. Be your own advocate. You’re not being paranoid - you’re being smart.
Mark Alan
February 3, 2026 AT 19:23jonathan soba
February 5, 2026 AT 17:05It’s interesting how the article cites 13% incidence at >300mg, yet ignores the confounding variable of concurrent stimulant use - caffeine, nicotine, even over-the-counter decongestants. The real risk isn’t venlafaxine alone; it’s the cumulative sympathetic burden. Most patients aren’t screened for lifestyle factors. The drug isn’t the villain - it’s the context.
matthew martin
February 6, 2026 AT 17:54Man, this hit different. I was on venlafaxine for a year - felt like a new person mentally. But my wife kept nagging me to check my BP. I rolled my eyes. Then I did - 152/98. I didn’t even know what that meant until I Googled it.
Turns out I was one of those ‘no symptoms’ cases. We switched to escitalopram. My mood stayed stable. My BP? Back to 118/76.
It’s wild how your brain feels better while your body screams in silence. Pay attention to the quiet stuff. It’s usually the loudest.
Irebami Soyinka
February 8, 2026 AT 01:56Y’all in the West always think your meds are magic. Here in Nigeria, we use herbs, diet, and prayer - and guess what? Our hypertension rates are lower than yours, even without SSRIs. You pop pills like candy and wonder why your heart is broken. This drug is not a cure - it’s a Band-Aid on a gunshot wound.
And now you’re surprised your BP is up? 🤦♀️
Maybe stop blaming the medicine and look at your stress, your sugar, your sleep - and your soul.
doug b
February 9, 2026 AT 08:31Mel MJPS
February 9, 2026 AT 10:14Thank you for writing this. I was terrified to speak up about my BP rising on venlafaxine because I didn’t want to seem ungrateful - like I was complaining about the thing that saved my mental health. But I’m so glad I did. My doctor listened. We lowered the dose and added a tiny bit of lisinopril. I’m still on the med, but now I’m safe. You’re not choosing between mind and heart. You can have both. Just don’t go silent.