Bariatric Surgery and Medication Absorption: How Weight Loss Surgery Changes Your Drug Doses
 Jan, 29 2026
Jan, 29 2026
Bariatric Medication Adjustment Calculator
Medication Adjustment Tool
This calculator estimates dose adjustments needed after bariatric surgery based on the type of procedure and medication.
Recommended Adjustment
Important Safety Notice
What Happens to Your Medicines After Bariatric Surgery?
If you’ve had or are considering bariatric surgery, you might not realize how deeply it changes the way your body handles medicine. It’s not just about losing weight-it’s about your whole digestive system being rewired. After surgery, pills that used to work perfectly might stop working at all. Or worse, they might work too well and cause side effects. This isn’t rare. In fact, up to 68% of people who have Roux-en-Y gastric bypass need their medications changed within the first year.
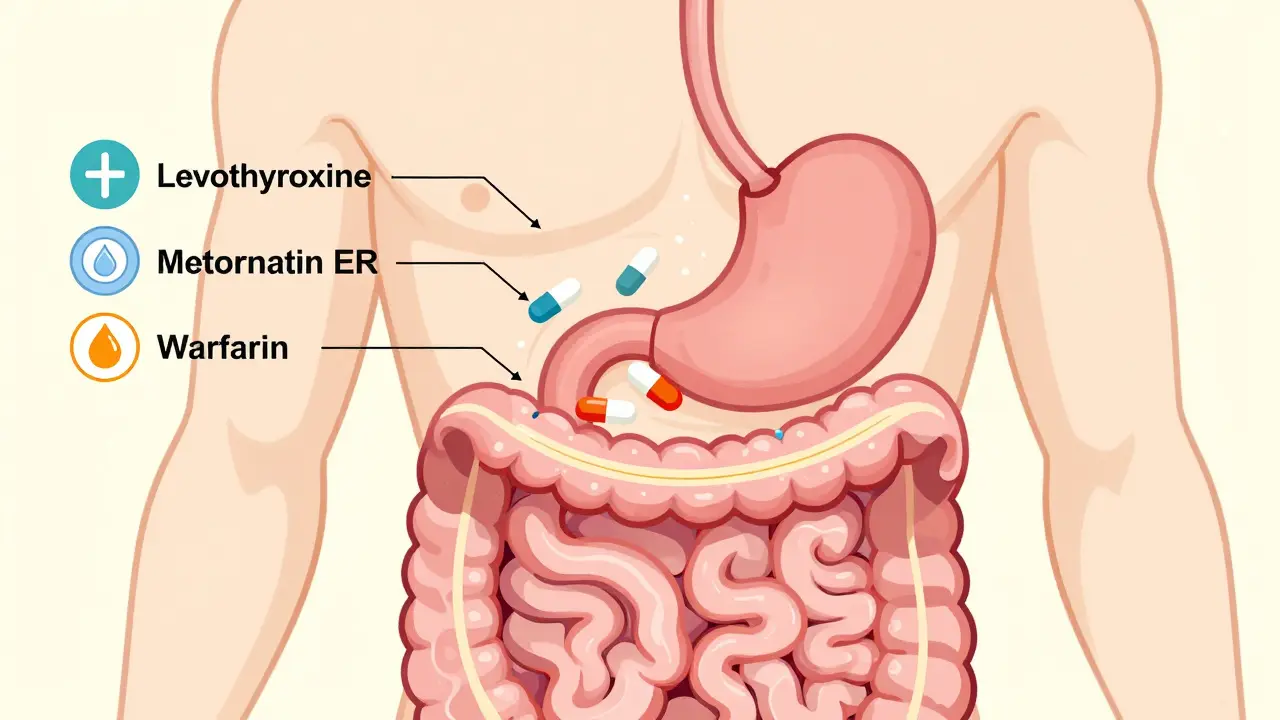
Why? Because the stomach and intestines are no longer the same. Surgeons shrink your stomach, skip parts of your small intestine, and change how food-and drugs-move through your body. The result? Your body absorbs medications differently. Some drugs get absorbed too fast. Others don’t get absorbed at all. And if you’re taking something like warfarin, levothyroxine, or metformin ER, even a small change can be dangerous.
How Different Surgeries Change Drug Absorption
Not all bariatric surgeries are the same-and neither are their effects on medication. The two most common procedures today are sleeve gastrectomy and Roux-en-Y gastric bypass (RYGB). Each affects drug absorption in distinct ways.
Sleeve gastrectomy removes about 80% of your stomach, leaving a narrow tube. Your duodenum (the first part of the small intestine) stays intact, so most drugs still pass through the usual absorption zones. But because your stomach is smaller and produces less acid, pills may not dissolve properly. Gastric pH rises from around 2 to 5, which messes with drugs that need acid to break down, like ketoconazole or iron supplements. Still, overall absorption stays fairly close to normal for most medications.
Roux-en-Y gastric bypass is where things get complicated. A small stomach pouch is created, and the duodenum is bypassed entirely. Food and drugs now travel directly into the middle of the small intestine, skipping the area where most drugs are absorbed. This bypass can be 100-150 cm long-roughly a quarter of your entire small intestine. That’s a massive loss of absorption surface. Studies show this surgery reduces absorption of calcium by 35%, levothyroxine by 25-30%, and extended-release pills by 40-60%.
Even rarer procedures like biliopancreatic diversion with duodenal switch cause even more dramatic changes, cutting absorption by 50-70% for many drugs. But because only about 2.5% of patients get this surgery, most concerns focus on sleeve and bypass.
Why Extended-Release Pills Often Fail
One of the biggest problems after bariatric surgery? Extended-release (ER) or controlled-release medications. These pills are designed to slowly release their contents over hours, traveling the full length of your gut. After RYGB, they don’t have time to do that.
Instead of dissolving gradually, they shoot through your shortened pathway too quickly. The result? You get a burst of drug all at once-or worse, none of it at all. Mayo Clinic data shows that 47% of time-release medications stopped working properly after RYGB. Common culprits include:
- Metformin ER - plasma levels drop by 30-40%
- Glipizide XL - efficacy falls by 50-75%
- Oxycodone CR - bioavailability drops 60%
- Levothyroxine ER - absorption plummets without switching to immediate-release
Doctors now recommend switching all ER pills to immediate-release versions right after surgery. For example, if you were taking 500 mg of metformin ER once daily, you’d switch to 500 mg of regular metformin twice daily. The total daily dose stays the same, but now your body has a chance to absorb it properly.

What About Liquid Medications and Timing?
For the first 3 months after surgery, liquid or crushed medications are often preferred. Pills can get stuck in the tiny stomach pouch or fail to dissolve. Liquid forms bypass that problem entirely.
Timing also matters. Acid-dependent drugs like itraconazole or rilpivirine need low pH to dissolve. Take them with food, and they won’t work. Take them 30-60 minutes before eating, and absorption improves by up to 22%, according to University of Florida research.
Lipophilic drugs-those that dissolve in fat-like cyclosporine or certain antidepressants, need bile and fat to be absorbed. After RYGB, bile mixing is reduced, so taking these with a small amount of fat (like a tablespoon of peanut butter or a few almonds) can make a big difference.
Drugs That Need Close Monitoring
Some medications have such narrow safety margins that even small changes in absorption can cause toxicity or treatment failure. The American Society for Metabolic and Bariatric Surgery (ASMBS) recommends therapeutic drug monitoring for 12 high-risk classes:
- Anticoagulants (warfarin)
- Antiepileptics (phenytoin, valproic acid)
- Immunosuppressants (cyclosporine, tacrolimus)
- Thyroid hormone (levothyroxine)
- Antidepressants (sertraline, fluoxetine)
- Antidiabetics (insulin, sulfonylureas)
For warfarin, 60% of RYGB patients need a 25-35% dose increase. One study found patients went from 5 mg daily to 8 mg daily within 6 months. Without monitoring, they could’ve bled internally or developed a clot.
Levothyroxine is another major issue. Patients often report feeling tired, gaining weight, or having brain fog-even when their TSH was stable before surgery. The fix? Switch to immediate-release levothyroxine, take it on an empty stomach, and check TSH every 6-8 weeks until stable. Many patients need a 20-50% dose increase.
What Patients Are Really Saying
Real-world experiences confirm the science. In online communities like r/bariatricsurgery, users share stories of failed meds:
- “I took 75 mcg of levothyroxine for years. After RYGB, I gained 15 pounds in 3 months. My endocrinologist upped me to 125 mcg. Within 2 weeks, I had energy again.”
- “My pain pills stopped working after surgery. I had to switch from oxycodone CR to regular oxycodone every 4 hours. My surgeon said it was normal.”
- “I was told to crush my pills. One time I forgot and swallowed a whole metformin ER tablet. It came out whole in my stool. I was terrified.”
A 2022 survey found that 78% of community pharmacists felt unprepared to handle post-bariatric medication questions. And 63% had seen at least one case of treatment failure directly linked to absorption issues.
In New Zealand, Medsafe recorded 142 adverse drug reactions in bariatric patients between 2018 and 2022. Over half involved blood thinners, diabetes meds, or painkillers. The most common complaints? “Pills not dissolving,” “meds not working,” and “having to take more pills than before.”
What You Should Do Now
If you’re scheduled for surgery:
- Ask your surgeon for a referral to a clinical pharmacist who specializes in bariatric care.
- Bring a full list of all medications, supplements, and over-the-counter drugs you take.
- Ask: “Which of my meds need to be switched to immediate-release? Which need dose changes?”
- Don’t assume your prescriptions will stay the same.
If you’ve already had surgery:
- Review your meds with your pharmacist every 3 months for the first year.
- Watch for signs your meds aren’t working: fatigue, mood changes, unexplained weight gain, irregular heartbeat, or pain returning.
- If you notice pills coming out whole in your stool, tell your doctor immediately.
- Use liquid or crushed forms if you’re still in the early post-op phase.
Many hospitals now use a 5-step assessment tool to evaluate medication risks after surgery. It checks drug properties, surgical type, and patient history. This simple system reduced readmissions by 34% in UK hospitals.
The Future of Bariatric Medication Management
Change is coming. The FDA now requires new oral drugs to include bariatric surgery absorption data in their labels. The European Medicines Agency made it mandatory in January 2024.
New technologies are emerging too. Intarcia’s ITCA 650-tiny implant that delivers exenatide under the skin-works perfectly after RYGB, unlike oral versions. pH-adaptive capsules, still in trials, dissolve only in the right intestinal environment, no matter the stomach pH. And AI-powered dosing calculators, now used in 83 U.S. hospitals, predict the right dose based on your surgery type, weight, and lab values.
Soon, pharmacogenomics may play a role too. Mayo Clinic is testing whether your genes (like CYP2C9 or CYP2C19 status) can help predict how you’ll respond to meds after surgery. Early results suggest dosing accuracy improves by 30% when genetics are combined with anatomy data.
One thing is clear: bariatric surgery isn’t just a weight-loss tool. It’s a metabolic reset that changes how your body processes medicine. Ignoring that fact puts your health at risk. The right adjustments don’t just make your meds work-they can save your life.
Do all bariatric surgeries affect medication absorption the same way?
No. Sleeve gastrectomy mainly reduces stomach size and acid production, so absorption changes are moderate. Roux-en-Y gastric bypass bypasses parts of the small intestine, causing major drops in absorption-especially for extended-release drugs. Biliopancreatic diversion causes the most severe changes. The key factor is whether the duodenum is bypassed. If it is, expect significant drug absorption changes.
Can I still take my extended-release pills after bariatric surgery?
Most experts strongly advise against it. Extended-release pills rely on long transit times through the intestines. After bypass surgery, they move too quickly and don’t release properly. Many patients report seeing whole pills in their stool. Switching to immediate-release versions is standard practice. Your pharmacist can help you find the right equivalent dose.
How do I know if my medication isn’t working after surgery?
Watch for symptoms that return or worsen. If you’re on levothyroxine and suddenly feel tired or gain weight, your dose may be too low. If you’re on warfarin and notice bruising or bleeding, your INR might be too high. For diabetes meds, rising blood sugar levels without dietary changes are a red flag. Always check with your doctor and ask for therapeutic drug monitoring if you’re on a high-risk medication.
Should I crush my pills after surgery?
Only if your doctor or pharmacist says it’s safe. Some pills-especially extended-release or enteric-coated ones-should never be crushed. Crushing them can release the full dose at once, causing overdose. For example, crushing oxycodone CR can be deadly. Always check the label or ask a pharmacist before crushing any medication.
How often should I get my blood tested after bariatric surgery?
For high-risk drugs like warfarin, phenytoin, or cyclosporine, testing should start within 2-4 weeks after surgery and continue weekly until stable. After that, monthly checks for 3-6 months, then quarterly. For thyroid hormone (levothyroxine), check TSH every 6-8 weeks until levels are steady. Calcium, vitamin D, and iron should be checked every 3-6 months indefinitely.
Jason Xin
January 30, 2026 AT 11:58Yanaton Whittaker
January 31, 2026 AT 15:34Kathleen Riley
February 2, 2026 AT 14:44Holly Robin
February 2, 2026 AT 17:11Shubham Dixit
February 4, 2026 AT 14:08KATHRYN JOHNSON
February 5, 2026 AT 01:46Sazzy De
February 5, 2026 AT 08:28Gaurav Meena
February 7, 2026 AT 07:34