Crohn’s Disease: Managing Chronic Inflammation with Biologic Therapy
 Dec, 16 2025
Dec, 16 2025
When you have Crohn’s disease, your body turns against itself. The immune system doesn’t just fight off germs-it attacks the lining of your gut, causing painful inflammation, ulcers, and sometimes life-threatening complications. Unlike occasional stomach bugs, this isn’t something that clears up with rest or antacids. It’s a lifelong condition that flares up without warning, making daily life unpredictable. But over the last 25 years, a new class of drugs called biologic therapies has changed the game. These aren’t your grandfather’s pills. They’re precision-targeted treatments that stop inflammation at its source.
What Exactly Is Crohn’s Disease?
Crohn’s disease is one type of inflammatory bowel disease (IBD). It doesn’t just affect one part of your digestive tract-it can show up anywhere from your mouth to your anus. Most often, it hits the end of the small intestine (the terminal ileum) and the beginning of the colon. The inflammation isn’t surface-deep. It goes all the way through the intestinal wall, which is why complications like strictures (narrowing), fistulas (abnormal tunnels), and abscesses happen so often. About 30-50% of people with Crohn’s develop strictures within 10 years. Around 25-35% end up with fistulas.
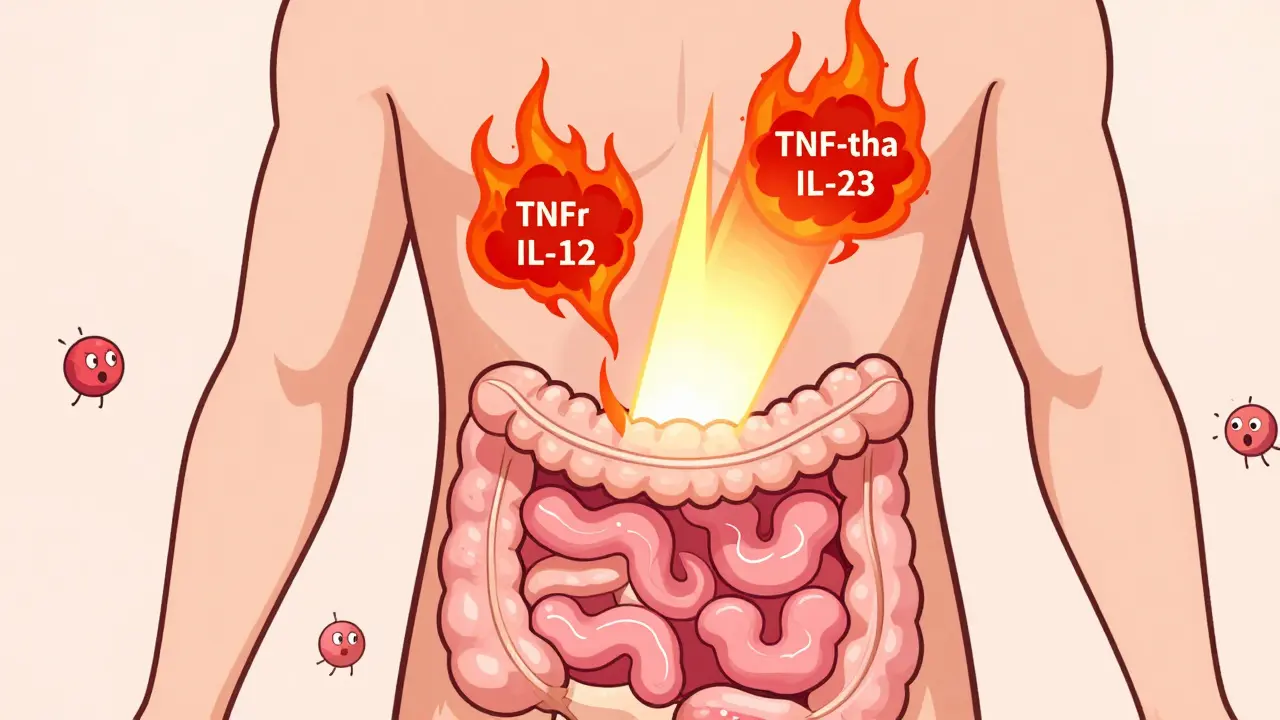
It’s not caused by bad food or stress, though those can make symptoms worse. The real culprit is a mix of genetics, immune misfires, and environmental triggers. Over 200 genes have been linked to Crohn’s, with the NOD2 gene mutation found in 30-40% of people with a family history. Your immune system sees harmless gut bacteria as enemies and launches a full-scale attack. White blood cells flood the area, releasing inflammatory chemicals like TNF-alpha, IL-12, and IL-23. These are the exact targets of modern biologic drugs.
Why Conventional Treatments Often Fall Short
For decades, doctors relied on steroids like prednisone to calm flares. But steroids are like fire extinguishers-you use them in emergencies, not every day. Long-term use leads to bone loss, weight gain, diabetes, and mood swings. Immunosuppressants like azathioprine or methotrexate help, but they take months to work and don’t heal the gut lining. Studies show only 20-30% of patients achieve mucosal healing with these drugs. That means the inflammation is still there, quietly damaging tissue, even if symptoms seem under control.
Biologics changed that. They don’t just suppress the whole immune system. They hit specific molecules driving the inflammation. And they work faster. While traditional drugs might take 3-6 months to show results, biologics can start reducing symptoms in just 2-4 weeks.
The Biologic Arsenal: What’s Available Today
There are now five anti-TNF drugs approved for Crohn’s: infliximab (Remicade), adalimumab (Humira), certolizumab pegol (Cimzia), golimumab (Simponi), and their biosimilars like Inflectra. These block TNF-alpha, the main inflammatory signal in Crohn’s. About 30-40% of patients go into remission with these drugs, compared to 15-20% on placebo.
But TNF isn’t the only player. Vedolizumab (Entyvio) works differently. Instead of shutting down inflammation everywhere, it stops immune cells from even getting into the gut. It’s like putting up a gate at the entrance. Only 25% of immune cells go to the intestines, so it’s much safer for people worried about infections elsewhere. It’s slower to work-10 to 14 weeks-but has lower rates of antibody formation (just 4% vs. 15-20% for anti-TNFs).
Then there’s ustekinumab (Stelara). It blocks IL-12 and IL-23, two key cytokines involved in the Th17 pathway. In clinical trials, 34-44% of patients reached remission at 8 weeks. At one year, about half still stayed in remission. That makes it a strong option for people who didn’t respond to anti-TNFs.

Choosing the Right Biologic: It’s Not One-Size-Fits-All
There’s no magic formula for picking the best biologic. But experts have some clear guidelines. If you have severe disease, deep ulcers, or perianal fistulas, starting with a biologic right away (called “top-down” therapy) cuts your risk of needing surgery by 50% over five years. That’s huge.
For most people, anti-TNF drugs like adalimumab or infliximab are the first choice. But if you have other autoimmune conditions like psoriasis or multiple sclerosis, vedolizumab is often preferred because it’s gut-specific and doesn’t affect the brain or skin. Ustekinumab is a good backup if anti-TNFs fail or cause side effects.
Cost matters too. Annual prices range from $35,000 for adalimumab to over $70,000 for ustekinumab. Biosimilars are cheaper-sometimes 30% less-and just as effective. Insurance approval can take weeks, so planning ahead is key.
Therapeutic Drug Monitoring: The Secret Weapon
One of the biggest mistakes patients make? Assuming once you start a biologic, you’re good to go. But many people lose response over time-not because the drug stopped working, but because their body made antibodies against it or they weren’t getting enough of it in their blood.
That’s where therapeutic drug monitoring comes in. Doctors check your drug levels in the blood. For infliximab, the target range is 3-7 μg/mL. For adalimumab, it’s 5-12 μg/mL. If you’re below that, your dose can be increased or given more often. If you’re above, you might be at higher risk for side effects. Studies show patients who get their levels checked are 3.5 times more likely to stay in remission.
This isn’t optional anymore. It’s standard care at major IBD centers. Skipping these tests is like driving blindfolded.
Real People, Real Experiences
On Reddit’s r/Crohns_Disease forum, one user said infliximab cut his bowel movements from 15 a day to 2 after just three infusions. Another developed a lupus-like reaction after 18 months on Humira and spent six months recovering with steroids.
A 2023 survey of over 1,200 patients found 78% felt their quality of life improved on biologics. Many got back to work, stopped needing hospital stays, and stopped relying on steroids. But 65% said cost was a major problem. Four in ten delayed doses because copays were over $150 per injection or infusion.
Side effects happen. About 35% report injection or infusion reactions-itching, flushing, chills. Around 28% worry about long-term infection risks. And 22% struggle with the logistics: scheduling infusions around work, remembering injections, dealing with insurance paperwork.

What Happens Before You Start?
Before your first biologic, you’ll need a few tests. A TB screening (Quantiferon Gold test) is required because these drugs can reactivate latent tuberculosis. Hepatitis B and C tests are also standard. Your heart function may be checked, especially if you’re older or have a history of heart issues.
If you’re on a subcutaneous biologic like Humira or Cimzia, you’ll learn how to self-inject. Most people get the hang of it after two or three supervised sessions. Nurses walk you through it-how to store the pen, where to inject (thigh or belly), how to handle any redness or swelling at the site.
Infusion centers are different. You sit for an hour or two while the drug drips in. Nurses watch for reactions. You’ll get pre-meds like antihistamines or steroids to prevent headaches or chills.
What’s Coming Next?
The future of Crohn’s treatment is getting even more precise. Ozanimod (Zeposia), a pill that traps immune cells in lymph nodes, showed 37% remission rates in trials. Mirikizumab, which blocks just the IL-23p19 subunit, achieved 40% endoscopic improvement. These drugs could offer new options for people who’ve tried everything else.
Biosimilars are already lowering costs. By 2030, they could cut biologic prices by 15-30%. That means more people will have access. But the real breakthrough will come from combining treatments-using biologics with diet, microbiome therapies, or even stem cell transplants in extreme cases.
Living Well on Biologics
Biologics don’t cure Crohn’s. But they can turn it from a life-disrupting illness into a manageable condition. People on these drugs report fewer hospital visits, more energy, and the ability to travel, work, and plan families.
Success isn’t just about feeling better. It’s about healing the gut. Mucosal healing-where the lining of the intestine actually repairs itself-is the real goal. Biologics achieve that in 40-60% of patients, compared to 20-30% with older drugs.
Stay on top of your monitoring. Don’t skip blood tests. Talk to your IBD nurse specialist. Use apps like MyIBDCoach to track symptoms. Join a support group. And if cost is a barrier, ask about patient assistance programs. Many cover 30-50% of out-of-pocket costs.
Crohn’s disease doesn’t define you. With the right treatment, you can live a full, active life. The tools are here. The science is proven. You just need to use them wisely.
Can biologics cure Crohn’s disease?
No, biologics cannot cure Crohn’s disease. They manage the condition by reducing inflammation and inducing remission. Many patients stay in remission for years, but the disease remains active at a cellular level. Stopping treatment often leads to flare-ups. The goal is long-term control, not a permanent cure.
How long does it take for biologics to work?
It varies by drug. Anti-TNF agents like infliximab and adalimumab usually start working in 2-4 weeks. Vedolizumab takes longer-10 to 14 weeks-because it works by blocking immune cell movement rather than directly neutralizing cytokines. Full benefits often take 3-6 months. Patience is key, but if there’s no improvement by 12 weeks, your doctor may adjust your plan.
Are biologics safe for long-term use?
Biologics are generally safe for long-term use, but they do carry risks. The biggest concern is serious infections-like tuberculosis, pneumonia, or sepsis-because they suppress parts of the immune system. The risk is about 12-15 infections per 100 patient-years, compared to 8-10 with older drugs. Regular screenings and monitoring reduce these risks significantly. Cancer risk is slightly elevated but remains low overall.
What happens if a biologic stops working?
Loss of response is common, especially with anti-TNF drugs. It can happen due to antibody formation or low drug levels. Your doctor will check your blood levels and test for antibodies. If levels are low, you may get a higher dose or more frequent infusions. If antibodies are present, switching to a different biologic-like moving from an anti-TNF to vedolizumab or ustekinumab-is often the next step. Many patients respond well to a switch.
Can I stop biologics if I feel better?
Most doctors advise against stopping biologics even if you feel fine. Stopping increases the risk of relapse by up to 70% within a year. Some patients may try tapering under close supervision, but this is rare and only done in cases of deep, sustained remission with documented mucosal healing. Never stop on your own-always discuss it with your gastroenterologist first.
How do I afford biologics if they’re so expensive?
Many pharmaceutical companies offer patient assistance programs that cover 30-50% of out-of-pocket costs for eligible patients. Biosimilars are significantly cheaper than brand-name drugs and are just as effective. Ask your doctor or pharmacist about these programs. Some nonprofits and foundations also provide grants for IBD patients. Insurance prior authorizations can be frustrating, but IBD nurse specialists can help navigate the process.
Janelle Moore
December 17, 2025 AT 06:20Henry Marcus
December 17, 2025 AT 07:54Carolyn Benson
December 17, 2025 AT 10:48Chris porto
December 18, 2025 AT 21:41William Liu
December 19, 2025 AT 01:57Aadil Munshi
December 19, 2025 AT 12:04Frank Drewery
December 19, 2025 AT 13:30Danielle Stewart
December 20, 2025 AT 00:30mary lizardo
December 20, 2025 AT 17:01jessica .
December 20, 2025 AT 21:33Ryan van Leent
December 21, 2025 AT 19:33Sajith Shams
December 22, 2025 AT 16:18Adrienne Dagg
December 23, 2025 AT 23:28Erica Vest
December 24, 2025 AT 02:25