Statin Intolerance: What to Do When Muscle Pain Keeps You From Taking Your Cholesterol Medicine
 Dec, 15 2025
Dec, 15 2025
For millions of people, statins are a lifeline. They cut LDL cholesterol by up to 60%, slashing heart attack and stroke risk. But for some, the cost is muscle pain - aching thighs, stiff shoulders, weakness that makes climbing stairs feel like a marathon. When this happens, many stop taking their statin. And that’s where things get dangerous.
Is It Really the Statin?
Not always. The biggest myth about statin intolerance is that muscle pain equals statin damage. In reality, most muscle symptoms people blame on statins aren’t caused by them at all. The landmark SAMSON trial found that 90% of side effects patients reported - including muscle pain, fatigue, and brain fog - happened just as often when they were taking a sugar pill. That’s the nocebo effect: if you expect to feel bad, your brain finds a way to make it happen. Real statin-associated muscle symptoms (SAMS) are rare. The National Lipid Association says true intolerance means you couldn’t tolerate two different statins: one at the lowest dose, another at any dose. And even then, symptoms must disappear when you stop the drug and return when you restart it. Only about 34% of people who think they’re intolerant actually meet that standard. Many people confuse statin pain with ordinary aches. Osteoarthritis affects 41% of those labeled statin-intolerant. Vitamin D deficiency? Present in 29%. Fibromyalgia? Seen in 18%. Even viral infections or overtraining can mimic statin side effects. A 2022 study showed that when doctors used the official NLA criteria, misdiagnosis dropped from 68% to just 22%.What Does Real Statin Muscle Pain Feel Like?
If it’s truly SAMS, the pain isn’t sharp or localized. It’s usually:- Proximal - feels in your thighs, buttocks, shoulders, or lower back
- Symmetric - both sides of your body feel it
- Slow to start - comes on within 30 days of starting or increasing the dose
- Described as heaviness, stiffness, or cramps - not sudden, stabbing pain
Why Some Statins Hurt Less Than Others
Not all statins are created equal. Lipophilic statins - like simvastatin and atorvastatin - easily slip into muscle cells. That’s why they’re more likely to cause muscle symptoms. Hydrophilic statins - like pravastatin and rosuvastatin - stay mostly in the liver, where they’re meant to work. Studies show hydrophilic statins have 28% lower rates of muscle complaints. If you had trouble with simvastatin, switching to rosuvastatin might be the answer. Even low-dose atorvastatin (10mg) is tolerated by 89% of people who couldn’t handle higher doses. Dosing matters too. Taking a statin every other day, or even once a week (like 600mg rosuvastatin weekly), can cut LDL by nearly half in many people - with far fewer side effects. It’s not a cure-all, but it’s a tool many doctors overlook.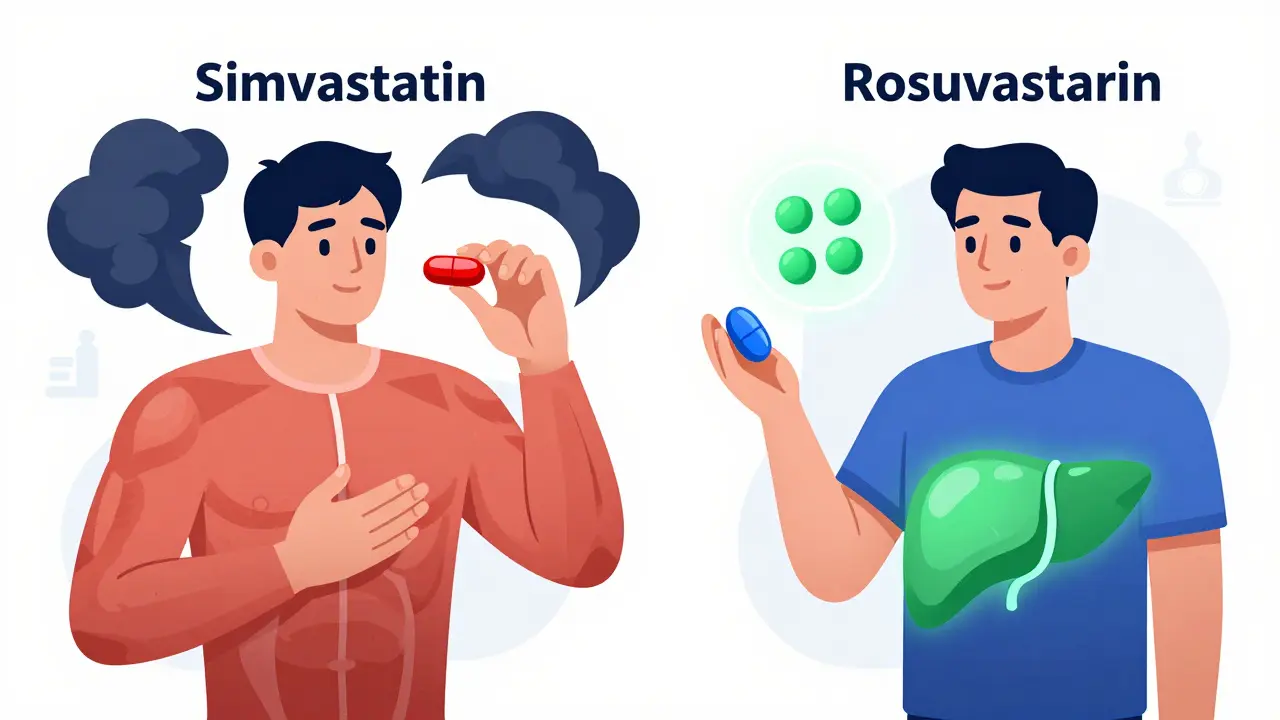
What to Try When Statins Won’t Work
If you’ve truly tried two statins and still have symptoms, you’re not out of options. Here’s what works:- Ezetimibe (10mg daily): Blocks cholesterol absorption in the gut. Lowers LDL by 18%, with 94% of people tolerating it well. Often paired with a low-dose statin if you can tolerate even a little.
- Bempedoic acid (180mg daily): Works in the liver like statins but doesn’t enter muscle cells. Reduces LDL by 17%, with 88% tolerability. Also lowers heart attack risk in high-risk patients.
- Bile acid sequestrants (e.g., colesevelam): Bind cholesterol in the gut. Cut LDL by 15-18%, but can cause bloating and constipation in 22% of users.
- PCSK9 inhibitors (evolocumab, alirocumab): Injected every 2-4 weeks. Lower LDL by up to 60%. Used in patients with very high risk - like those with genetic high cholesterol or prior heart attacks. Adherence is 91% in trials. Cost is high ($5,800/year), and insurance often requires prior authorization - 37% of requests get denied.
- Inclisiran: A new shot given just twice a year. Lowers LDL by 50%. Approved in 2023. Still expensive, but easier to stick with than daily pills.
What About CoQ10 or Natural Remedies?
Coenzyme Q10 (CoQ10) is often recommended because statins lower its levels in the body. But here’s the truth: double-blind trials show only 34% of people report feeling better on CoQ10 - and there’s no proof it reduces muscle damage. It might help some, but don’t count on it. Fish oil? Great for triglycerides, not LDL. Red yeast rice? Contains natural statins - same risks, no regulation. Turmeric? No meaningful cholesterol effect. There’s no magic supplement. Stick with proven, FDA-approved therapies. Natural doesn’t mean safe or effective.
Why Stopping Statins Is Riskier Than You Think
The biggest danger isn’t muscle pain. It’s what happens when you quit. People who stop statins because of muscle symptoms have a 25% higher chance of having a heart attack or stroke within a year, according to JAMA Cardiology. That’s not a small risk. It’s life-changing. A 2023 study of 12,000 patients found that those who stopped statins due to muscle complaints had the same long-term heart risk as people who never took them. But here’s the kicker: 71% of those patients said they were terrified of having a heart attack after quitting. The solution isn’t to suffer through pain. It’s to find the right alternative. With the right approach, over 90% of people labeled “statin intolerant” can reach their LDL goals without side effects.What to Do Next
If you’re struggling with muscle pain on statins:- Don’t quit cold turkey. Talk to your doctor first.
- Ask if you’ve tried two different statins - one at the lowest dose.
- Get your vitamin D and thyroid checked. Deficiencies are common culprits.
- Request a rechallenge: stop the statin for 4-6 weeks. If symptoms vanish, restart a different one. If they come back, you have true intolerance.
- Ask about ezetimibe or bempedoic acid as first-line alternatives.
- If your risk is high (family history, prior heart event, diabetes), ask about PCSK9 inhibitors or inclisiran.
Can statins cause permanent muscle damage?
No. Statin-related muscle symptoms are almost always reversible. Once you stop the statin, muscle pain, weakness, and stiffness typically fade within days to weeks. True muscle damage - like rhabdomyolysis - is extremely rare and only happens with very high CK levels and other signs like dark urine. Even then, with prompt treatment, full recovery is common.
Why do some people tolerate statins and others don’t?
Genetics play a big role. A variant in the SLCO1B1 gene - especially the *5 and *15 alleles - makes it harder for the body to clear certain statins from muscle tissue, increasing the risk of side effects. People with this variant are 4.5 times more likely to have muscle pain. Testing for this gene is not routine yet, but it’s becoming more common in high-risk patients. Other factors include age, kidney or liver function, drug interactions (like with antibiotics or grapefruit juice), and thyroid problems.
Is it safe to take statins every other day?
Yes, for many people. Studies show that taking rosuvastatin 600mg once a week lowers LDL by nearly half - similar to daily dosing. The same works for atorvastatin or simvastatin at lower doses. This approach reduces side effects while still offering strong heart protection. It’s not for everyone - especially those with very high cholesterol or a history of heart attack - but it’s a valid option if your doctor agrees.
Can I switch from a statin to a PCSK9 inhibitor without trying other options first?
Generally, no. Guidelines recommend trying ezetimibe or bempedoic acid first. These are oral, affordable, and effective for many. PCSK9 inhibitors are reserved for those who can’t reach their LDL goal with other drugs, or who have very high risk (like familial hypercholesterolemia or prior heart events). Insurance usually requires you to fail at least one oral option before approving the injectable.
How long does it take to find the right alternative therapy?
Most people need 3 to 6 months to find the right combination. It’s not a quick fix. You might try one drug, wait 6-8 weeks to see how it works, adjust the dose, then try another. Real-world data shows patients average 2.3 different strategies before reaching their target LDL. Patience and persistence pay off - and you’re not alone. Thousands have walked this path before you.
Kitty Price
December 16, 2025 AT 02:29sue spark
December 16, 2025 AT 20:08Randolph Rickman
December 18, 2025 AT 11:03Kayleigh Campbell
December 19, 2025 AT 07:19Dave Alponvyr
December 19, 2025 AT 19:56Josias Ariel Mahlangu
December 20, 2025 AT 16:49Colleen Bigelow
December 20, 2025 AT 19:14Billy Poling
December 21, 2025 AT 21:22James Rayner
December 23, 2025 AT 04:27Arun ana
December 24, 2025 AT 08:49Kim Hines
December 25, 2025 AT 12:37Cassandra Collins
December 27, 2025 AT 09:33Aditya Kumar
December 28, 2025 AT 19:48